Dietetic interns are required to write an article in the graduate-level advanced nutrition course about a topic that is of interest to their selected audience. These articles are published here so that our students' interests can be explored and the quality of their work observed. Browse the topics below:
Beverages
How Not To Be a Caffeine Zombie
Christian Fant, Dietetic Intern 2019

My personal story with caffeine addiction was just realized not too long ago and I wanted to quit the dirty high just like all of you. It was causing me to be a caffeine zombie. Some of my symptoms were frequent urination all through the night, insomnia, disordered sleep patterns, elevated heartrates in the gym, fatigue, and tiredness throughout the day. I had headaches if I tried to stop cold turkey. Does this sound like some of the things you're going through? If so, I've got some great things for you to add to your regime to kick this caffeine addiction.
How Does Caffeine Work?
Caffeine is an interesting little fellow. Seems innocent enough right? I mean the FDA states 400 mg is safe for adults, so what's the big deal? The big deal is that caffeine is a drug, and with drugs come addiction and dependence. Ninety percent of Americans use caffeine daily and 50% of those people are getting at least 300mg a day (About Caffeine, n.d.). With those statistics, I guess that if you're reading this you're one of those people. So how does it work? Caffeine is absorbed in the small intestine, and then crosses the blood-brain barrier which blocks the absorption of adenosine in our brain cells. Adenosine is a nucleoside and neurotransmitter. The blockage of adenosine blunts fatigue and tiredness which is a wanted effect by those of us who drink caffeinated drinks. Dopamine, the feel-good hormone, also works more effectively when adenosine is blocked, which causes a high feeling. This increases the likelihood of the addiction aspect. Once this process starts, the body adapts and increases the number of adenosine receptors in the brain to compensate for all this caffeine floating around. This means more caffeine needs to be consumed to get the same blockage of adenosine to blunt fatigue and tiredness. This is also called building up a tolerance to caffeine. So, if caffeine is blocking adenosine in the brain it just disappears and goes away right? Sadly no. Excess adenosine floating around cues the adrenal glands to release adrenaline and cortisol causing increase blood sugar, elevated heart rate, and increased blood pressure. This is an unnecessary stress response on the body that is abused day in and day out with caffeine junkies. When you already have a stressful life, this is not something you want to add to the mix of things. So, what is a person to do?
Well, fear not because I'm going to arm you with a caffeine kickin' tool belt. You wouldn't go into battle without the right tools, so don't battle your caffeine addiction without the right tools either. My tool belt consists of supplements and strategies to fight caffeine addiction, reduce inflammation, and decrease unwanted stress.
Use of Adaptogens
Adaptogens are plant herbs and roots that have been shown to reduce stress. This is important because adaptogens benefit the HPA-axis system, which stands for hypothalamic, pituitary, adrenal axis. It's a domino effect that starts like this:
The hypothalamus in the brain signals the pituitary glands, which then stimulate the adrenal glands to produce the stress hormones. Chronic stress keeps this system engaged longer than it should, and caffeine can play a major role in this. Ashwagandha is an adaptogen that has been proven to reduce stress, anxiety, and lower cortisol. A 2012 study involved 64 participants who had chronic stress. The participants either took a placebo or 300 mg of full-spectrum highly concentrated extract of ashwagandha for 60 days (Chandrasekhar, Kapoor, & Anishetty, 2012). The results showed a decrease in cortisol and fewer stress results from stress tests in the group taking ashwagandha. Adding ashwagandha to your caffeine kicking regimen can help you start the recovery process of decreasing stress and regulating your stress hormones.
Fish Oil
If you're eating the standard American diet you are probably lacking in omega-3 fatty acids and getting abundant omega-6 fatty acids from oils. Fish oil, a great omega-3 source, not only has been shown to reduce inflammation but also has been shown to lower cortisol and adrenaline levels. A study with 7 healthy men showed a decrease in epinephrine and cortisol levels after stress from just 3 weeks of fish oil supplementation (Delarue, et al., 2003). Decreasing unnecessary inflammation and cortisol production from the adrenal glands is going to help with the overstressed state your body is in with caffeine. I recommend reducing your total intake of omega-6 sources, which include vegetable oils and fried foods, and increasing your omega-3's through fish oil supplementation or through eating more fatty fish like salmon and tuna.
Sleep
Sleep is more important than we realize. Insomnia is at the cornerstone of being chronically stressed and overworked. Fixing your circadian rhythm of sleep is a major part of not being a caffeine zombie, and large amounts of caffeine are hindering this normal rhythm from occurring. Studies have shown that caffeine up to 6 hours before bedtime can disrupt normal circadian sleep patterns (Drake, Roehrs, Shambroom, & Roth, 2013). Step 1 of fixing your sleep is to not consume caffeine close to your bedtime. When your sleep is altered this way, it changes your cortisol balance, and remember, cortisol is the stress hormone that we don't want to be elevated all the time. Normal cortisol production should be highest in the morning and lowest in the evening before bed. An overworked adrenal gland from caffeine causes too much cortisol production in the evening altering the normal balance. This makes a person feel unrested and tired in the morning and have insomnia at night. This can be fixed by maintaining healthy sleep hygiene. Melatonin can be a great supplement to help initiate sleep hygiene if needed. Studies have shown that 5-10 grams of melatonin about an hour or two before bed every night decreases the amount of time it takes to fall asleep, and helps you stay asleep longer (Dahlitz, et al., May 1991; Oldani, et al., 1994).
Caffeine Weaning
Quitting caffeine cold turkey is usually ineffective for most people long term and causes unwanted side effects like headaches and extreme fatigue. Since you are a caffeine junkie your body is used to having an increased amount of adenosine receptors that are not naturally obtained without the use of caffeine. Your body wants the amount of caffeine you have been subjecting it to over the past weeks, months, and years. This must be gradually decreased to completely avoid withdrawal symptoms. Caffeine weaning has been shown in studies to be the most effective way to quit a case of caffeine dependency (W.H.G, 2014). A case study from Australia studied the effects of caffeine weaning on a 50-year-old woman with a 35-year history of over 350 mg of caffeine a day. During the first week, her intake was around 160 mg, the second week 80 mg, and then the 3rd week to the 8th week, 35 mg. After this process, she was able to quit her caffeine addiction. My recommendations are to cut your caffeine intake in half each week until you get low enough that you feel like you can quit.
How To Make It All Work
The most important part of this process is quitting the caffeine addiction and controlling stress. Without cessation of caffeine over time none of these supplements I listed as part of your toolbelt can help. If you're taking over 400 mg of caffeine on most days of the week from energy drinks, coffee, and sodas, the rest of these tips won't be effective. It's an all or nothing strategy. Start with the caffeine weaning! Once you do that, then supplement with ashwagandha, fish oil, and melatonin daily. This will help jumpstart you in the right direction to reducing stress, getting better sleep, controlling cortisol, and managing your caffeine addiction and all the damage it's caused!
References
About Caffeine. (n.d.). Retrieved from https://www1.villanova.edu/villanova/studentlife/health/promotion/goto/…
Chandrasekhar, K., Kapoor, J., & Anishetty, S. (2012). A prospective, randomized double-blind, placebo-controlled study of safety and efficacy of a high-concentration full-spectrum extract of Ashwagandha root in reducing stress and anxiety in adults. Indian Journal of Psychological Medicine,34(3), 255. doi:10.4103/0253-7176.106022
Dahlitz, M., Alvarez, B., Vignau, J., English, J., Arendt, J., & Parkes, J. (may 1991). Delayed sleep phase syndrome response to melatonin. The Lancet,337(8750). doi:org/10.1016/0140-6736(91)92787-3
Delarue, J., Matzinger, O., Binnert, C., Schneiter, P., Chioléro, R., & Tappy, L. (2003). Fish oil prevents the adrenal activation elicited by mental stress in healthy men. Diabetes & Metabolism,29(3), 289-295. doi:10.1016/s1262-3636(07)70039-3
Drake, C., Roehrs, T., Shambroom, J., & Roth, T. (2013). Caffeine effects on sleept 0, 3, or 6 hours before going to bed. Journal of Clinical Sleep Medicine. doi:10.5664/jcsm.3170
Head, K. A., ND, & Kelley, G. S., ND. (2009). Nutrients and botanicals for treatment of stress: Adrenal fatigue, neurotransmitter imbalance, anxiety, and restless sleep. Alternative Medicine Review,14, 2nd ser., 114-140. Retrieved from http://archive.foundationalmedicinereview.com/publications/14/2/114.pdf
Lipman, F., Dr. (2018, November 07). Adaptogens: Nature's miracle anti-stress and fatigue fighters. Retrieved from https://www.bewell.com/blog/adaptogens-natures-miracle-anti-stress-and-fatigue-fighters/
Neville, A., Dr. (n.d.). Desperate for shut-eye? This sleep hormone holds the key. Retrieved from https://www.healing.org/symptoms/insomnia/
Oldani, A., Ferini-Strambi, L., Zucconi, M., Stankov, B., Fraschini, F., & Smirne, S. (1994). Melatonin, and delayed sleep phase syndrome. NeuroReport,6(1), 132-134. doi:10.1097/00001756-199412300-00034
Stromberg, J. (2013, August 09). This is how your brain becomes addicted to caffeine. Retrieved from https://www.smithsonianmag.com/science-nature/this-is-how-your-brain-becomes-addicted-to-caffeine-26861037/
W, H. G. (2014). A case study investigating a behavioural intervention to reduce caffeine consumption. Journal of Women's Health Care,03(05). doi:10.4172/2167-0420.1000186
Is Your Coffee Obsession Healthy? Maybe.
Shelbie Calk, Dietetic Intern 2017

Most Americans start the day with a cup of coffee, and we aren't alone! In fact, roughly 80% of the adult population worldwide consumes coffee on a regular basis (Komes & Busic, 2014). For most of us, coffee is our major source of caffeine to help us power through the day. However, lately I have heard several of my friends on social media and in conversation mention that they are trying to stop drinking coffee. Some of my friends have even tried replacing their morning cup of joe with warm, lemon water. But, why? Any time I ask for a reason, they always just simply say, "because I've always heard coffee isn't good for you." As an avid coffee drinker, I have decided to make it a personal mission to debunk the myths and spread knowledge I have learned through my own obsessive research about the true nature of coffee and its perceived health effects. Coffee has been recognized for its various health benefits for over 1000 years! As early as fourth century BC, coffee was used as a mood stabilizer and often even given as a prescription for various illnesses (Bizzo, Farah, Kemp, Scancetti, 2015). Coffee is a blend of many different bioactive compounds that have varying effects on the body.
What Are These Bioactive Compounds?
First and foremost, caffeine. Caffeine is the most well-known compound found in coffee, and is also the reason most of us drink this delicious brew in the first place. Caffeine is a heat-stable alkaloid that stimulates the central nervous system, acting as an adenosine-receptor antagonist (Bae, Park, Im, Song, 2014). In simple terms, this means that caffeine binds to certain receptors in the brain, blocking the effects of adenosine. Adenosine is a compound that signals to our brain that it is time for sleep. When caffeine binds instead of adenosine, we feel energized and ready to take on the day! Caffeine also functions to enhance mood, improve exercise performance, and has even shown to decrease tremors in individuals with Parkinson's disease (Esquivel & Jimenez, 2012). You might also be surprised to find that coffee is actually full of antioxidants! In some countries, coffee is actually the major source of antioxidants for the general population (Komes & Busic, 2014). A class of phenolic compounds called chlorogenic acids are the main bioactive components responsible for coffee's abundant antioxidant activity. Several studies have reported that chlorogenic acids found in coffee are greatly associated with a decreased risk of diabetes, Parkinson's, Alzheimer's Disease, and even liver cancer (Komes & Busic, 2014). Over the years, researchers have also found that brewed coffee demonstrates a significant oxygen scavenging ability. However, longer roasting periods can result in a total loss of chlorogenic acid, and overall antioxidant activity. Therefore, medium-roasted coffee tends to have the highest oxygen scavenging ability, or the highest concentration of antioxidants (Komes & Busic, 2014).
Trigonelline is an alkaloid compound found in coffee and is largely responsible for coffee's bitter taste. Trigonelline has been shown to regenerate dendrites and axons in the brain, which may help to improve memory (Farah, 2012). Through the brewing process, trigonelline is converted to nicotinic acid, or a B-vitamin known as Niacin. Essentially, niacin helps the body to utilize the energy in our food (Komes & Busic, 2014).
Cafestol and Kahweol are also major bioactive compounds in coffee. Both compounds are diterpenes, which have shown to be help protect against liver damage as well as prevent premature cell death resulting from neurotoxins produced from Parkinson's disease (Bae, et al. 2014; Kim & Lee, 2015).
Coffee has also shown to be neuroprotective. Researchers believe that this is due partly to caffeine and caffeic acid. Certain studies have found that caffeic acid protects against amyloid ß induced neurotoxicity and tau phosphorylation, which means that coffee can possibly decrease the risk of Alzheimer's disease and help to support cognition through old age (Kim & Lee, 2015).
All of these health benefits sound amazing, right? Does all of this prove that coffee is in fact good for everyone? Well, no. Of course not. That would be too simple. Whether or not you experience positive effects from coffee all depends on how your body processes it!
The caffeine in coffee is metabolized by an enzyme in the liver, resulting from the gene CYP1A. Variations in the CYP1A gene affect how quickly you metabolize caffeine. Do you ever wonder why some people are anxious and jittery after just one cup of coffee, while others still struggle to keep their eyes open after 3 or 4 cups? Well, the answer lies in your genetics! Variations in the CYP1A gene place each of us in one of two groups: "fast" metabolizers vs "slow" metabolizers. Individuals with the "fast" CYP1A gene metabolize coffee roughly 4 times faster than individuals with the "slow" metabolizing variant (O'Connor, 2016). So how does that affect the health benefits mentioned previously? Well, several research studies have found that for "slow" metabolizers, many of the perceived health benefits of coffee consumption seem to actually have an opposite effect. Moderate to high coffee consumption among "slow" metabolizers has been associated with a higher risk of heart attack, heart disease, hypertension, and a lack of "protective" effects against some cancers when compared to those with the "fast" metabolizing variation of CYP1A (Cornelis, et al. 2006; Kressor, 2016).
Approximately 50% of the population has the genotype to be considered "slow" metabolizers. With a country divided, this could definitely explain the immense amount of conflicting data surrounding coffee consumption related to overall health. Obviously, not all of us are able to be tested for which CYP1A genotype we have. My best advice? Listen to your body! If you think you are a "fast" metabolizer, go ahead and stumble out of bed each morning to pour yourself a big cup of warm, delicious coffee. If you aren't sure which group you fall into, just be sure to listen to your body! If you don't feel like you tolerate coffee very well, then it might be better to err on the side of caution and minimize your caffeine intake.
1. Bae, J., Park, J., Im, S., & Song, D. (2014). Coffee and health. Integrative Medicine Research, 3(4), 189-191. https://doi.org/10.1016/j.imr.2014.08.002
2. Cornelis, M. C., El-Sohemy, A., Kabagambe, E. K., & Campos, H. (2006). Coffee, CYP1A2 Genotype, and Risk of Myocardial Infarction. Jama,295(10), 1135. doi:10.1001/jama.295.10.1135
3. Esquivel, P., & Jiménez, V. M. (2012). Functional properties of coffee and coffee by-products ?. FRIN, 46(2), 488-495. https://doi.org/10.1016/j.foodres.2011.05.028
4. Farah, A. (2012). Coffee: Emerging Health Effects and Disease Prevention, First Edition. Y.F. Chu (Ed.) Blackwell Publishing Ltd.
5. Kim, J., & Lee, K. W. (2015). Neuroprotective, 423-427. https://doi.org/10.1016/B978-0-12-409517-.00046-2
6. Komes, D., & Busic, A. (2014). Antioxidants in Coffee, 25-32. https://doi.org/10.1016/B978-0-12-404738-9.00003-9
7. Kresser, C. (2016, December 15). Coffee is good for you-unless it's not! Retrieved April 21, 2017, from https://chriskresser.com/coffee-is-good-for-you-unless-its-not/
8. Letícia, M., Bizzo, G., Farah, A., & Kemp, J. A. (2015). Highlights in the History of Coffee Science Related to Health. Coffee in Health and Disease Prevention. Elsevier Inc. https://doi.org/10.1016/B978-0-12-409517-5.00002-4
9. O'Connor, A. (2016, July 12). For Coffee Drinkers, the Buzz May Be in Your Genes. Retrieved April 21, 2017, from https://well.blogs.nytimes.com/2016/07/12/for-coffee-drinkers-the-buzz-may-be-in-your-genes/?_r=0
Grape Expectations: Is Red Wine Actually Cardioprotective?
Heather Rose Anderson, Dietetic Intern 2018

Introduction
Red wine's association with cardiovascular disease is a very popular topic. This is because cardiovascular disease is so prevalent in the world and not to mention, is the number one cause of death in the United States with 633,842 deaths in 2016 according to the Centers for Disease Control.1 This means that one in every four deaths is a cardiovascular event. Due to red wine's widely ranged consumption, there has been multiple studies supporting that it prevents cardiovascular disease. But, is that true? Health care and medical professionals are one of the primary people translating "overheard" and/or "small talk" information regarding nutrition to patients, so it is pertinent to deliver the correct advice to the right population. With not much time to do research themselves, here is up-to-date information for those in need of a quick answer that is easy to deliver to other medical professionals and patients who inquire. So, here we go! Let's get started with this:
The French Paradox
Have you ever heard friends or family say while they are topping off their cabernet, "Hey, wine is good for the heart?" Well, this impression of wine and heart health surfaced in the late 1980's due to the French Paradox. Although controversial, high intakes of saturated fat have been shown to be positively related to high mortality from coronary artery disease. However, the situation in France, shown by French epidemiologists, reveals much different data. The French Paradox refers to the idea that drinking wine might help explain the low rates of heart disease among the French, regardless of their high intake of dietary cholesterol and saturated fat. The epidemiological studies showed that consumption of alcohol at the level of intake in France, about 20-30 grams per day, can reduce risk of coronary artery disease by at least 40%.2,3 Therefore, this French Paradox may not be so "paradoxical" after all. Now that we've covered the background story of wine and cardiovascular health, we can move on to the gooey details.
What Is in Red Wine That Could Make It Cardioprotective?
Red wine contains polyphenols. Typically, a five-ounce glass of red wine contains around 100 mg of polyphenols.3 Polyphenols are secondary metabolites of plants and are usually involved in the defense against ultraviolet radiation or attack by pathogens, but recently research has consistently shown to offer protection against cardiovascular disease.4,5 Polyphenols contribute to the bitterness, astringency, color, flavor, odor and oxidative stability. If you've ever sipped a glass of red wine, you may have experienced the taste of bitterness and/or acidity - those are polyphenols! These polyphenols originate in the grape berry. If you didn't know, wine is made from grapes - specifically white wine is made from white grapes and red wine is made from red grapes. White wine, however, does not share the same properties with their red wine counterparts. White wines typically do not have polyphenols which are shown to be cardioprotective and those that do contain a very small amount - not enough to impact the health of someone's heart. Now let's dig a little deeper. To start, there are more than 8,000 polyphenolic compounds identified.5 In red wine, resveratrol is the existing polyphenol carrying out these cardioprotective effects.6,7 The health benefits of this polyphenol, resveratrol, as an antioxidant is continually emerging in research.
What Does the Research Say?
It is suggested that a moderate intake of alcohol (1 drink for a woman and 2 drinks for a man) lowers your risk for developing cardiovascular disease.8 As you know, cardiovascular disease is when there is a buildup of sticky plaque in the arteries of the blood vessels or "the highways" in your heart. This build up is called atherosclerosis. Atherosclerosis is an inflammatory process.9 Due to alcohol's perceived positive effect on cardiovascular disease, it is theorized that alcohol consumption affects inflammation. There are labs that doctors can look at that tell if your body is in a state of inflammation, putting you at risk for developing cardiovascular disease - these labs are fibrinogen and C-reactive protein. If these labs are too high, then it could indicate inflammation. After three weeks of drinking 150 mL (a little over a half of a cup) of red wine a day, C-reactive protein stayed the same and fibrinogen improved significantly. To note, fibrinogen improvement also means there is an increase in blood clotting due to the platelet-to-platelet binding during platelet aggregation which could be something to watch in certain patient populations.10 Additionally, during these 3 weeks, there were also positive changes in total cholesterol and triglycerides, both indicative of a positive impact on your heart's health.11 Out of 136,382 people, a significant inverse association between light-to-moderate wine drinking and vascular risk was also shown in another study. This showed that with light-to-moderate wine drinking of around 1-2 drinks per day, your risk for vascular disease (arteries) decreased drastically.
But not so fast. With emerging genetic evidence, research from the University of Gothenburg showed that only about 15% of the human population with the specific form of the cholesteryl ester transfer protein (CETP) gene actually gain this positive cardiovascular benefit from moderate alcohol consumption.12 Genetics has been playing an underrated role in our health in the past. We now know not to discuss health in absolutes. If you think about it, how many of the "rules" we follow (e.g., don't eat red meat and/or don't eat fat because it makes you fat) are deterring on our genetic makeup?
What does drinking a glass of wine have to do with genetics anyways? Patients with the genotype (CETP) are known to reduce their risk of heart disease; however, two distinct groups were looked at based on whether they had the B1 or B2 version of this CETP gene in the Gothenburg study. The B2 version exhibited a lower risk of cardiovascular disease in patients who enjoyed moderate alcohol consumption. Out of the 618 patients, only 19% of them had this B2 version.
Genetic testing is increasingly becoming more and more common and could be pertinent to any mutations in a person's genes that may cause or progress illness or disease. But what if a patient or client does not have the funds or interest to get a genetic test? Well, there are other ways to tell that wine and/or alcohol consumption may not be right for your patient. According to the Mayo Clinic, signs such as flushing, hives, runny nose, migraines, low blood pressure, nausea, vomiting and/or diarrhea are signs of alcohol intolerance. Alcohol intolerance occurs when the body does not have the right enzymes to break down the toxins in alcohol - this is caused by inherited (genetic) traits. Any signs of alcohol intolerance are enough evidence to refrain from drinking because there may be a genetic predisposition to these toxins.
Conclusion
To say red wine is cardioprotective is one of those "absolute health" statements I mentioned above. First and foremost, listening to the body to determine alcohol tolerance is essential. Secondly, genetic testing to determine if one has the right version of the alcohol-related CETP gene which shows to be cardioprotective is the most proficient way of determining if wine is cardioprotective for an individual.
References
1. National Center for Health Statistics. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm. Published March 17, 2017. Accessed April 17, 2018.
2. Ferrieres J. The French paradox: lessons for other countries. Heart. 2004;90(1):107-111. doi:10.1136/heart.90.1.107.
3. Renaud S, Lorgeril MD. Wine, alcohol, platelets, and the French paradox for coronary heart disease. The Lancet. 1992;339(8808):1523-1526. doi:10.1016/0140-6736(92)91277-f.
4. Bonnefont-Rousselot D. Resveratrol and Cardiovascular Diseases. Nutrients. 2016;8(5):250. doi:10.3390/nu8050250
5. Pandey K.B., Rizvi SI. Plant Polyphenols as Dietary Antioxidants in Human Health and Disease. Oxidative Medicine and Cellular Longevity. 2009;2(5):270-278. doi:10.4161/oxim.2.5.9498.
6. D'Archivio M, Filesi C, Varì R, Scazzocchio B, Masella R. Bioavailability of the Polyphenols: Status and Controversies. International Journal of Molecular Sciences. 2010;11(4):1321-1342. doi:10.3390/ijms11041321.
7. Showing all foods in which the polyphenol Resveratrol is found Food Composition. (n.d.). Retrieved March 29, 2018, from http://phenol-explorer.eu/contents/polyphenol/592
8. Castelnuovo AD. Meta-Analysis of Wine and Beer Consumption in Relation to Vascular Risk. Circulation. 2002;105(24):2836-2844. doi:10.1161/01.cir.0000018653.19696.01.
9. Ross, R. (1999). Atherosclerosis--an inflammatory disease. The New England Journal of Medicine, 340(2), 115-126. https://doi.org/10.1056/NEJM199901143400207
10. Brunner, E. (2010). Fibrinogen and Clotting Factors. In Encyclopedia of Stress (pp. 51-55). https://doi.org/10.1016/B978-012373947-6.00159-8
11. Retterstol L, Berge KE, Braaten Ø, Eikvar L, Pedersen TR, Sandvik L. A Daily Glass Of Red Wine: Does It Affect Markers Of Inflammation? Alcohol and Alcoholism. 2005;40(2):102-105. doi:10.1093/alcalc/agh132.
12. Barter PJ. Cholesteryl ester transfer protein (CETP). AccessScience. January 2003. doi:10.1036/1097-8542.900195.
13. Alcohol Consumption and Genetics. Psych Central. https://psychcentral.com/lib/alcohol-consumption-and-genetics/. Published July 17, 2016. Accessed April 22, 2018.
14. Alcohol intolerance. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/alcohol-intolerance/symptoms-causes/syc-20369211. Published March 26, 2015. Accessed April 22, 2018.
Why Your A1C Isn’t The “Tell-all” of Your Glucose Control
Regan Hawkins, Dietetic Intern 2022
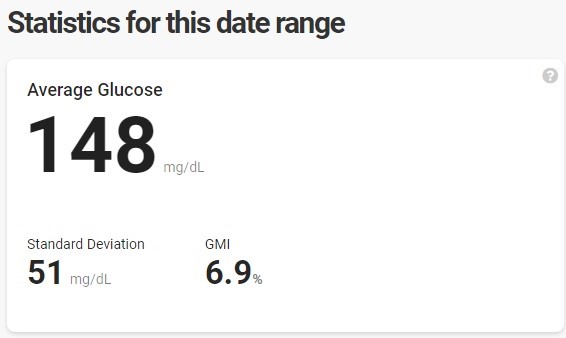
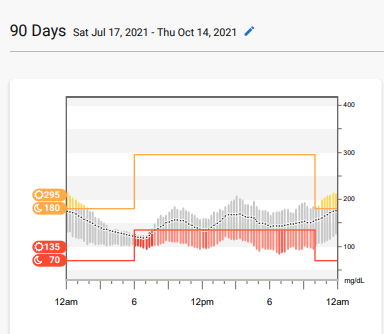
Living with type 1 diabetes for the past 22 years, I have been taught that my A1C is the “tell-all” of my health. Interestingly enough, the older I have gotten, the more I realize that is not completely true. At my last endocrinology appointment, I went in just waiting for a lecture about how my A1C had increased since my last visit. I was a 5.6% at my last appointment and whole-heartedly believed I crept up into the six’s since then. My hectic schedule had made my diabetes management suffer. I had to cancel my gym membership and quit meal prepping due to time constraints of being a grad student, dietetic intern, and still trying to work. Heck, I was proud when I had time to wash my hair or shave my legs! When my doctor came back into the room and told me my A1C was a 5.9%, I was in disbelief. This made me curious, so I went home and pulled up my CGM (continuous glucose monitor) report from my Dexcom. Unsurprisingly my report said that my A1C should have been around 6.9% - very different from what I was told at my appointment (see my CGM data below).
This concerned me because I want to stay healthy and live complication-free, but obviously, my diabetes management needs to be tweaked. Not everyone is fortunate and has access to a CGM, so this made me want to dive deeper into other ways to evaluate glucose control. If you are like me and want more in-depth information regarding your diabetes management, please keep reading!
What’s the deal with A1C?
For the most part, everyone who sees a health care professional to care for their diabetes knows that an A1C is what their doctor uses to measure glucose control. On the other hand, not everyone knows exactly what an A1C measures or what the numbers even mean. For those who do not - an A1C gives an average glucose level over a three-month period. The numbers given to us represent a three-month average glucose level. See the chart below:
The reason why this test is not the most reliable is that it is an average. There are several things that can affect this number including hypoglycemia, hyperglycemia, anemia, red blood cell turnover, pregnancy, etc. (American Diabetes Association, 2020). If you are having a rough time controlling your glucose and happen to be on the rollercoaster of highs and lows, this will cause the accuracy of your A1C to be swayed. We have been taught that the higher the A1C, the greater the chance of diabetic complications (American Diabetes Association, n.d.). So why only rely on one test to measure our compliance? This test is not sensitive to recent changes in diabetes management, so the use of other tests in conjunction is optimal. Fortunately, we have evolved and found new ways to determine how well we are managing our diabetes. Let’s talk about a few.
1,5-Anhydroglucitol – the more the merrier!
Glycomark is a new test that is starting to rise in popularity. This test measures the 1,5-Anhydroglucitol (1,5AG) in our bodies to give us a better idea of glucose control. This test is more sensitive to hyperglycemia and hyperglycemic excursions, aka fluctuations in blood glucose levels (Merendino, n.d.). Glucose and 1,5-AG circulate in the bloodstream in someone with well-controlled glucose levels. Both substances are filtered by the kidneys and are reabsorbed by the body. When someone has glucose levels >180mg/dL, which is the renal threshold, glycosuria (when urine contains more sugar than it should) will block the reabsorption of 1,5-AG. This results in low levels of 1,5-AG in the body due to the urinary excretion of the substance (Glycomark, n.d.). These findings resulted in the test called Glycomark, which measures serum 1,5-AG in the body. A low number will represent that the individual is experiencing hyperglycemia or hyperglycemic excursions. This test allows health care professionals to see snapshot of a patient’s glucose after meals. This can be measured every 1-2 weeks and is sensitive to recent changes in medication.
In a study performed by Dungan et al., (2006), two patients had their CGM data compared side by side. Patient A had an A1C of 7.43% and a 1,5-AG of 12.37μg/ml. Patient B had an A1C of 7.27% and a 1,5-AG of 4.5μg/ml. If you were just comparing A1C, you would assume that patient B had a better value therefore they had better control. That would be incorrect. When examining CGM trends, patient B experienced several hyperglycemic excursions and did not stay within range (80-180mg/DL) for any length of time. Patient B’s CGM chart looked like a roller coaster with extreme ups and downs. Patient A’s CGM chart still had some highs and lows, but the trend was more level and stayed within range more of the time, which flattened the line trend. If the 1,5-AG value was used, it would be apparent that patient B was experiencing extensive glucose fluctuations.
Another study by McGill et al., (2004) found that 1,5-AG responded rapidly (within 2 weeks) to changes in diabetes therapy. Whereas no change was seen with A1C until week 4. With this being said, it just goes to show that A1C does not need to be our only indicator of the success of our diabetes therapy.
Continuous Glucose Monitor –our best friend
The biggest perk of having a CGM is the ability to see glucose trends. It gives us the luxury of seeing how things like exercise, stress, food, pregnancy, menstruation, illness, etc. affect our glucose. This is something we could not see unless we pricked our fingers 100+ times a day. Not everyone is lucky enough to have a CGM, but those who do should utilize all the tools that it provides. One of the free tools provided by a CGM is a GMI (glucose management indicator). The GMI will estimate what your A1C should be when you have blood work done and is a number that is provided by all CGMs. It does this by using the average glucose calculated from the last 12 days of CGM readings (Dexcom, n.d.). This, like 1,5-AG, allows us to see rapid changes in diabetes therapy, and if using the CGM alone and not the GMI, allows us to get real-time feedback.
Fructosamine and Glycated Albumin – the sweet proteins
According to Danese et al., (2015), the American Diabetes Association has recognized that certain patients with unreliable A1C values, as discussed above, need alternative means to measure average glucose. These alternative measures include the measurement of glycated albumin (GA) and fructosamine. Fructosamine is formed when glucose and protein combine and glycated albumin is the measurement of albumin that has been glycated (Shafi et al., 2013). These markers are not influenced by anemia or other conditions such as chronic kidney disease (Krhač, M. & Lovrenčić, 2019). Albumin is the most plentiful serum protein in the human body. Because of this, fructosamine is predominantly a measurement of GA. Levels of GA and fructosamine both increase when glucose concentrations increase and the proteins have a lower half-life of 14-21 days, as compared to hemoglobin with 90-120 days. This makes fructosamine and GA a good marker to assess glucose control over an intermediate time frame.
To sum it all up:
The main purpose of this discussion was to educate you on the importance of not just relying on your A1C but using other methods to help manage your diabetes. A1C is just a general snapshot and is used by most healthcare professionals who are checking labs. It is important to educate ourselves about the constantly evolving technology that affects our diabetes management. We must be advocates for ourselves and work with our health care providers to use accurate testing to manage our condition. Using the tools discussed can help fine-tune your diabetes management and give you a more detailed snapshot of what your glucose is doing, and not just guessing. Be your best advocate and talk to your healthcare provider about optimizing your diabetes management!
References
American Diabetes Association. (2020). 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2020. Diabetes care, 43(Supplement 1), S14-S31.
American Diabetes Association. (n.d.). Understanding A1C. Understanding A1C | ADA. Retrieved October 16, 2021, from https://www.diabetes.org/a1c.
Bergenstal, R. M., Beck, R. W., Close, K. L., Grunberger, G., Sacks, D. B., Kowalski, A., ... & Cefalu, W. T. (2018). Glucose management indicator (GMI): a new term for estimating A1C from continuous glucose monitoring. Diabetes care, 41(11), 2275-2280.
Danese, E., Montagnana, M., Nouvenne, A., & Lippi, G. (2015). Advantages and pitfalls of fructosamine and glycated albumin in the diagnosis and treatment of diabetes. Journal of diabetes science and technology, 9(2), 169-176.
Dexcom. (n.d.). What is Glucose Management Indicator (GMI)? Dexcom Continuous Glucose Monitor. Retrieved May 19, 2022, from https://provider.dexcom.com/what-glucose-management-indicator-gmi#:~:te….
Dungan, K. M., Buse, J. B., Largay, J., Kelly, M. M., Button, E. A., Kato, S., & Wittlin, S. (2006). 1, 5-anhydroglucitol and postprandial hyperglycemia as measured by continuous glucose monitoring system in moderately controlled patients with diabetes. Diabetes care, 29(6), 1214-1219.
Krhač, M., & Lovrenčić, M. V. (2019). Update on biomarkers of glycemic control. World journal of diabetes, 10(1), 1.
McGill, J. B., Cole, T. G., Nowatzke, W., Houghton, S., Ammirati, E. B., Gautille, T., & Sarno, M. J. (2004). Circulating 1, 5-anhydroglucitol levels in adult patients with diabetes reflect longitudinal changes of glycemia: a US trial of the GlycoMark assay. Diabetes Care, 27(8), 1859-1865.
Merendino, J. (n.d.). What is meant by the term excursion in diabetes patients? Sharecare. Retrieved May 5, 2022, from https://www.sharecare.com/health/diabetes/excursion-diabetes-patients#:….
Shafi, T., Sozio, S., Plantinga, L., Jaar, B., Kim, E., Parekh, R., Steffes, M., Powe, N., Coresh, J., & Selvin, E. (2013, May 15). Serum fructosamine and glycated albumin and risk of mortality and clinical outcomes in hemodialysis patients. American Diabetes Association. Retrieved May 20, 2022, from https://diabetesjournals.org/care/article/36/6/1522/33146/Serum-Fructos…
The glycomark test. Glycomark. (n.d.). Retrieved October 17, 2021, from https://glycomark.com/the-glycomark-test/.
Chronic Inflammation and Diabetes: Don’t Sugarcoat It
Reyes Banda, Dietetic Intern 2021

The Chicken or the Egg?
If you have been paying attention to the news lately you may have heard the term inflammation being thrown around. Inflammation is a complex mechanism that the body utilizes in response to some sort of irritation. This is known as acute inflammation. Acute inflammation is responsible for stopping intruders from entering our bodies. There is another side to the inflammation coin. This is known as chronic inflammation. Chronic inflammation is more of a slow burn in comparison to its acute counterpart. When it comes to diabetes and inflammation the question to ask, is what came first? Just like the chicken or the egg, diabetes or inflammation? Both conditions seem to overlap, but the main culprit is still at large. While the cause is still not completely understood, the truth of the matter is that both conditions are interconnected. Several models have been proposed as the root of the problem. These include obesity, diet, gut microbiome dysbiosis, sedentary lifestyle, air pollutants, vitamin D deficiency, genetic factors, and even oral health (Lontchi-Yimagou, 2013). While the main cause is still not completely understood, there is plenty of data linking inflammation to diabetes. Evidence linking inflammation and diabetes can be seen in a cohort study where inflammatory markers were measured between individuals with diabetes and individuals with no diabetes. The study showed that in subjects with no diabetes only 8.8% had markers above the median, while in diabetic subjects only 2.6% had no markers below the median (Duncan, 2003).
What to Look For?
If you are worried that inflammation may become an issue, the next time you visit your doctor mention this to them. Let them know about your concerns and ask them to check for inflammatory related markers. In 2004, researchers stated that excess adiposity is the most important risk factor for the development of insulin resistance and type 2 diabetes. In the study subjects with diabetes showed significantly higher levels of BMI, waist circumference, and waist-to-hip ratio. To add to these physical findings, diabetic subjects also reported lower levels of physical activity. The study’s main focus was measuring tumor necrosis factor (TNF)-α receptor 2, interleukin (IL)-6, and C-reactive protein (CRP) was higher in subjects with diabetes than in subjects with no diabetes (Hu, 2004). Although the best and most common indicator of inflammation in diabetics is HbA1c levels. HbA1c measures the average blood glucose level for the past ~90 days. Although sometimes controversial HbA1c is the gold standard for glycemic management. There are many links between poor glycemic control and inflammation markers. In 2006 study researchers found that among diabetic participants, higher levels of HbA1c were associated with higher levels of all three markers of inflammation, tumor necrosis factor-α receptor 2, interleukin-6, and C-reactive protein ( de Rekeneire, 2006).
Inflammation Complicates Diabetes Even More
You may be asking yourself what the consequences of inflammation are. Inflammation exacerbates all the complications that diabetes causes. The most common complications are diabetic retinopathy, diabetic neuropathy, diabetic nephropathy, and even metabolic disorders like hypertension. In studies, a link between diabetic retinopathy progression and inflammatory markers was established. Other links between inflammatory markers and microvascular and neural damage, and nephropathy progression have also been established (Navarro, 2005). Another complication that is not usually mentioned is the role that uncontrolled diabetes has on vascular health. Recent studies have found that activated leukocytes, which are inflammatory response cells, play a large role in capillary damage. Leukocytes after responding to chronic inflammation may linger in the body and cause heavier damage to even further vascular damage. Excess leukocyte entrapment and coagulation, induced by the vascular expansion may be a result of capillary occlusion and loss (Forrester, 2020).
Overall Dietary Patterns that Reduce Inflammation
So now that we know what inflammation is, how to measure inflammation, and the damage inflammation causes, there is only one question left to ask. How can I reduce my inflammation levels? As we learned earlier the main focus with inflammation and diabetes should always be blood glucose control. I want to discuss different foods that may help manage blood glucose levels and inflammation. There are many options one can use to maintain healthy blood glucose levels. A low carbohydrate approach or a more balanced Mediterranean Diet have shown great promise in glucose control. A “low carb” approach is usually delineated as a diet low in carbohydrates with an average consumption between 20 to 60 grams of carbohydrates per day. Trying to avoid foods that are high in carbohydrates might be a good place to start. Sugary beverages and desserts could be the beginning of this journey. Mediterranean diets are more balanced and usually include a wide variety of foods. In a Mediterranean diet, it is usually recommended to eat more vegetables, fruits, nuts, seeds, legumes, whole grains, herbs, spices, fish, seafood, and extra virgin olive oil. Usual Mediterranean diet recommendations also call for a restriction of sugary beverages, processed meat, refined grains, refined oils, and other highly processed foods. If you are looking for a small start to a low carb or Mediterranean diet you can start by including different ingredients like the ones mentioned above (Martín-Peláez et al, 2020).
Specific Foods that Reduce Inflammation
I want to show you some ingredients that can be easily added to your meals and can bring great benefits. In a recent study, avocado has shown beneficial effects by reducing oxidative and inflammatory stress. Avocados offer antioxidants known as phenolics that enhance blood flow and arterial health by inhibiting platelet aggregation. One-half avocado contains about 60 and 140 mg of gallic acid which are phenolic compounds and act as antioxidants (Dreher, 2013). Another approach that can be made is to increase nut intake. In a recent study, findings suggest that higher nut consumption may lead to lower CRP, lower plasma insulin, lower fasting blood glucose, and lower HbA1c levels (Mazidi, 2018). Eating a varied diet can help us introduce other food items that may be beneficial as well. In a recent study, dietary supplementation of blueberries decreased inflammatory markers like IL-6, IL-12, and CRP concentrations in individuals with low-grade inflammation (Kolehmainen et al., 2012). Another rich source of anti-inflammatory compounds is Cocoa. In 2014 study researchers gave diabetic patients 10g of cocoa twice a day for 6 weeks. Researchers found that Cocoa consumption lowered blood TNF-α and CRP, and IL-6 significantly (Parsaeyan, 2014).
Conclusion
Overall, diabetes is a complex disease. Poor glucose control seems to be the main cause of diabetic complications and the rise in inflammation. Diabetic complications will be worsened by inflammation. If you can manage blood glucose levels, you may be able to mitigate the damage. But, to truly measure the efficacy of the intervention, measuring inflammatory markers is a must. To help our body reduce inflammation it is advised we consume foods that are rich sources of antioxidants. Some dietary patterns have shown promise especially in reducing inflammation. The Mediterranean Diet has shown to be effective in reducing inflammation. The Mediterranean Diet includes a variety of ingredients that are high in antioxidant content while also reducing sources of inflammation like sugary beverages. Ingredients that may help reduce inflammation can be added to our daily dietary patterns. These ingredients like avocados or blueberries may be beneficial by reducing inflammation. If you have worries or concerns be sure to ask your dietitian and your doctor about inflammation during your next visits.
References
de Rekeneire N, Peila R, Ding J, Colbert LH, Visser M, Shorr RI, Kritchevsky SB, Kuller LH, Strotmeyer ES, Schwartz AV, Vellas B, Harris TB. (2006). Diabetes, hyperglycemia, and inflammation in older individuals: the health, aging and body composition study. Diabetes Care, 29(8):1902-8. doi: 10.2337/dc05-2327. PMID: 16873800.
Dreher, M. L., & Davenport, A. J. (2013). Hass Avocado Composition and Potential Health Effects. Critical Reviews in Food Science and Nutrition, 53(7), 738–750. https://doi.org/10.1080/10408398.2011.556759
Duncan, B. B., Schmidt, M. I., Pankow, J. S., Ballantyne, C. M., Couper, D., Vigo, A., Hoogeveen, R., Folsom, A. R., & Heiss, G. (2003). Low-Grade Systemic Inflammation and the Development of Type 2 Diabetes: The Atherosclerosis Risk in Communities Study. Diabetes, 52(7), 1799–1805. https://doi.org/10.2337/diabetes.52.7.1799
Forrester, J. V., Kuffova, L., & Delibegovic, M. (2020). The Role of Inflammation in Diabetic Retinopathy. Frontiers in Immunology, 11. https://doi.org/10.3389/fimmu.2020.583687
Hu, F. B., Meigs, J. B., Li, T. Y., Rifai, N., & Manson, J. E. (2004). Inflammatory Markers and Risk of Developing Type 2 Diabetes in Women. Diabetes, 53(3), 693–700. https://doi.org/10.2337/diabetes.53.3.693
Kolehmainen, M., Mykkänen, O., Kirjavainen, P. V., Leppänen, T., Moilanen, E., Adriaens, M., Laaksonen, D. E., Hallikainen, M., Puupponen-Pimiä, R., Pulkkinen, L., Mykkänen, H., Gylling, H., Poutanen, K., & Törrönen, R. (2012). Bilberries reduce low-grade inflammation in individuals with features of metabolic syndrome. Molecular Nutrition & Food Research, 56(10), 1501–1510. https://doi.org/10.1002/mnfr.201200195
Lontchi-Yimagou, E., Sobngwi, E., Matsha, T. E., & Kengne, A. P. (2013). Diabetes Mellitus and Inflammation. Current Diabetes Reports, 13(3), 435–444. https://doi.org/10.1007/s11892-013-0375-y
Martín-Peláez, S., Fito, M., & Castaner, O. (2020). Mediterranean Diet Effects on Type 2 Diabetes Prevention, Disease Progression, and Related Mechanisms. A Review. Nutrients, 12(8), 2236. https://doi.org/10.3390/nu12082236
Navarro, J. F., & Mora, C. (2005). Role of inflammation in diabetic complications. Nephrology Dialysis Transplantation, 20(12), 2601–2604. https://doi.org/10.1093/ndt/gfi155
Parsaeyan, N., Mozaffari-Khosravi, H., Absalan, A., & Mozayan, M. R. (2014). Beneficial effects of cocoa on lipid peroxidation and inflammatory markers in type 2 diabetic patients and investigation of probable interactions of cocoa active ingredients with prostaglandin synthase-2 (PTGS-2/COX-2) using virtual analysis. Journal of Diabetes & Metabolic Disorders, 13(1). https://doi.org/10.1186/2251-6581-13-30
Apple Cider Vinegar, Friend or Foe for Diabetes?
Lindsay Hetzel, Dietetic Intern 2017

Introduction
Apple cider vinegar has been on the forefront of discussion; everywhere we look there is chatter about how to take apple cider vinegar, what the benefits are, and who benefits from taking it. Researchers have discovered that the acetic acid in apple cider vinegar has been found to suppress body fat accumulation, leading scientists to find out what the other benefits the vinegar could provide (Kondo et al., 2009). From diving in to research to find these answers I have found that people with type II diabetes, obese individuals wanting to lose weight, and individuals with high cholesterol appear to benefit the most from ingesting apple cider vinegar. For the purpose of this article, individuals with diabetes will be the focus.
Vinegar has a long history, dating back to Babylonia 5,000 BC (Kondo et al., 2009). There are various types of vinegar consumed today, apple cider vinegar, rice wine vinegar, red and white wine vinegar, and balsamic vinegar used for seasoning and preserving food. The main component of vinegar is acetic acid derived from fermentation giving vinegar its distinctive taste and pungent smell (Budak et al., 2014).
Individuals with type II diabetes mellitus (T2DM) are growing in population due to rising obesity, diet choices, and genetics. There are an estimated 171 million people worldwide suffering with T2DM, and that number is expected to increase to 366 million by 2030 (Hlebowicz et al., 2007). Insulin resistance is a condition where the cells in our body do not accept the insulin our pancreas creates for us to utilize the glucose in our bloodstream, thus our cells become insulin resistant.
Experts conducting research have agreed on the dose on 30 ml of apple cider vinegar to be sufficient to see results (White et al., 2007) (Kondo et al., 2009) (Mitrou et al., 2015). A study of obese Japanese individuals were split in to 3 groups consuming 30 ml, 15 ml, or 0 ml of apple cider vinegar to identify if the effects of vinegar intake on the reduction of body fat (Kondo et al., 2009). After 12 weeks, both of the vinegar groups lowered their body weight, BMI, abdominal fat, waist circumference, and decreased serum triglyceride levels compared to the 0 ml group (Kondo et al., 2009). While both groups had success, the 30 ml group lost more weight than the low dose group, and maintained their weight loss better than the 15 ml group (Kondo et al., 2009).
Apple cider vinegar has positive effects on insulin sensitivity and natural honey has been shown to have positive effects on cardiovascular disease risk factors (Beheshti et al., 2012) (Derakhshandeh-Rishehri et al., 2014). Honey and vinegar are often combined to be able to tolerate the mixture. Iran has a traditional syrup composed of 1 kg honey, 1500 ml water, and 300 g of vinegar, and a few mint sprigs, known as Sekanjabin, one of the oldest Iranian drinks that was studied to evaluate the effects in healthy individuals measuring cardiovascular disease risk factors (Derakhshandeh-Rishehri et al., 2014). The group consuming the syrup had a negative result of increased fasting insulin levels, but decreased their total cholesterol (Derakhshandeh-Rishehri et al., 2014). Concluding, consuming this amount of honey and vinegar did not enhance, but did not worsen each other's effects.
Advantages for Type II Diabetes
Ingesting apple cider vinegar has been shown to raise insulin sensitivity when taken at mealtime and at bedtime (Johnston et al., 2004) (White et al., 2007). Research has shown in insulin-resistant study participants that consuming apple cider vinegar (20 grams) before a high carbohydrate meal such as a bagel with butter and orange juice, resulted in raising the whole-body insulin sensitivity after 1 hour in the participants by 34%, and increased satiety (Johnston et al., 2004) (Ostman et al., 2005).
Individuals with T2DM are aware of the "dawn-phenomenon" known as an abnormal rise in blood glucose in the early-morning hours (White, et al., 2007). Consuming 2 tablespoons (30 ml) of apple cider vinegar and 1 ounce of cheese before bedtime improved the blood glucose levels in the morning in individuals with T2DM (White et al., 2007). Acetic acid has an antiglycemic effect, reducing starch digestion and/or delaying gastric emptying (White et al., 2007).
Disadvantages for Type II Diabetes
Individuals with gastroparesis, or delayed gastric emptying resulting from type I or II diabetes typically suffer with nausea, bloating, and vomiting (Hlebowicz, 2007). Individuals with gastroparesis were found to be negatively effected after consuming vinegar, exasperating their delayed emptying even further, making it difficult to control their blood sugar (Hlebowicz, 2007).
Conclusion
Overall, apple cider vinegar is helpful and cost-effective for people with T2DM, wanting to lose weight, and decrease their cardiovascular disease risk factors. Consuming 30 ml of apple cider vinegar daily has been proven to improve health. Individuals with gastroparesis may want to skip the vinegar, due to worsening symptoms.
Disclosure: As always, consult your physician before beginning any new regimen.
Easy Apple Cider Vinegar Drink
1-2 tablespoons water
2 (30 ml) tablespoons apple cider vinegar
1/4 teaspoon honeyCombine and mix all ingredients. Optional add-ins: dash of cinnamon, few drops of lemon juice.
References
Beheshti, Z., Chan, Y., Sharif Nia, H., Hajihosseini, F., Nazari, R., Shaabani, M., & Omran, M. (2012). Influence of apple cider vinegar on blood lipids. Life Science Journal, 9(4). Retrieved from https://www.researchgate.net/profile/Hamid_Sharif_Nia/publication/26031….
Budak, N., Aykin, E., Seydim, A., Greene, A., & Guzel-Seydim, Z. (2014). Functional properties of vinegar. Journal of Food Science, 79(5). Retrieved from http://doi.org/10.1111/1750-3841.12434
Derakhshandeh-Rishehri, S., Heidari-Beni, M., Feizi, A., Askari, G., & Entezari, M. (2014). Effect of honey vinegar syrup on blood sugar and lipid profile in healthy subjects. International Journal of Preventative Medicine, 5(12), 1608-1615. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4336993/?report=printable
Hlebowicz, J., Darwiche, G., Bjorgell, O., & Almer, L. (2007). Effect of apple cider vinegar on delayed gastric emptying in patients with type 1 diabetes mellitus: a pilot study. BMC Gastroenterology, 7(46). doi:10.1186/1471-230X-7-46
Johnston, C.S., Kim, C.M., Buller, A.J. (2004). Vinegar improves insulin sensitivity to a high-carbohydrate meal in subjects with insulin reistance or type 2 diabetes. Diabetes Care, 27(1), 281-282. doi:10.2337/diacare.27.1.281
Mitrou, P., Petsiou, E., Papakonstantinou, E., Maratou, E., Lambadiari, V., Dimitriadis, P., … Spanoudi, F. (2015). The role of acetic acid on glucose uptake and blood flow rates in the skeletal muscle in humans with impaired glucose tolerance. European Journal of Clinical Nutrition, (69), 734-739. doi:10.1038/ejcn.2014.289
Ondo, T. K., Ishi, M. K., Ushimi, T. F., Gajin, S. U., & Aga, T. K. (2009). Vinegar Intake Reduces Body Weight , Body Fat Mass , and Serum Triglyceride Levels in Obese Japanese Subjects, 73(8), 1837-1843. http://doi.org/10.1271/bbb.90231
Ostman, E., Granfeldt, Y., Persson, L., & Bjorck, I. (2005). Vinegar supplementation lowers glucose and insulin responses and increases satiety after a bread meal in healthy subjects. European Journal of Clinical Nutrition, (59), 983-988. doi:10.1038/sj.ejcn.1602197
White, A. M., & Johnston, C. S. (2007). Vinegar ingestion at bedtime moderates waking glucose concentrations in adults with well-controlled type 2 diabetes. Diabetes Care, 30(11). Retrieved from DOI: 10.2337/dc07-1062
Diabetes with Disaster? 5 Supplements to Bring Some Disaster Relief to Your Life
Karlee Wright, Dietetic Intern 2020

The roller coaster of hyperglycemia to hypoglycemia and back up to hyperglycemia can be daunting and frustrating. The list of the many exhausting and strenuous effects of type 1 diabetes is endless. You spend months feeling under the weather and fatigued. Many doctors assume your diet is poor or you aren't taking your insulin properly, however, this is probably farthest from the truth.
You are trying various diets, exercise, adjusting your medication, and anything you have heard from your healthcare providers to control your diabetes, but it feels like the entire world is working against you. Sleep, hormones, stress, kids, work, money, anything, and everything can cause your blood sugar to fluctuate.
It is scary to think about neuropathy, high blood pressure, and possibly, end-stage renal disease if you can't get this under control. We need to stop this chaos! So... we ask... what's next? Have you thought about taking supplements? If so, why or why not? Is it a lack of knowledge? Overwhelmed by the different options? Well, let's discuss
The Chaos Ends Now
You are in control... 5 supplements...here we go...
1. CoQ10
2. Curcumin
3. Omega-3-Fatty Acids
4. Berberine
5. Benfotiamine
10 Out of 10 with CoQ10
When an individual has hyperglycemia with diabetes, impairments with oxidation, AKA, oxidative stress, can occur. Oxidative stress is when the body is not able to protect your cells and cells become damaged and can even lead to further damage to the organs. In the body, there are free radicals, and this is what can cause damage to the cells. Antioxidants are what protects the cells from free radicals. However, in diabetes antioxidants may be decreased. In a healthy individual, antioxidants are readily available, and glucose is processed at a steady rate (Bradley, 2007). However, with hyperglycemia, the body is trying to process more glucose and does not have antioxidants readily available. This causes excess free radicals, leading to dysfunction. Imagine a person blowing bubbles and trying to pop every single one of the bubbles before they pop or float away, STRESSFUL. An antioxidant that occurs naturally in the body is glutathione (GSH). For GSH to be produced in the body it needs glutaredoxins (Grxs) to function properly. Grxs are a group of proteins that help create GSH. However, when Grxs are produced in excess it can be an indicator of oxidative stress. Previous research has shown that Grxs are impaired in type 1 diabetes. (Montano et al., 2015).
A supplement that can reduce oxidative stress is CoQ10. CoQ10 is an antioxidant that naturally occurs in the body, however, may be depleted with diabetes. Research suggests 100 mg of CoQ10 two times a day lowered HbA1c, decreased Grx to normal levels, and lowered oxidative stress (Montano et al., 2015). The mechanism behind the action is the CoQ10 keeps the glucose processing steadily. Remember the bubbles; imagine blowing one bubble at a time and popping it, much easier and much less stressful.
It's a Win-Win with Curcumin
We discussed the oxidative stress that can occur with diabetes when we discussed the supplement, CoQ10. We know that the excess free radicals and lack of antioxidants cause oxidative stress. We also discussed how hyperglycemia can cause dysfunction within the cells. What we did not discuss is heme oxygenase (HO). HO is known to be an important part of the cellular defense, specifically, the cellular tissue is protected. HO is also associated with glucose metabolism and insulin release. Cells need to be healthy and working properly for the body to be well and to prevent further complications from occurring.
Curcumin is a compound found in turmeric. I am sure some of you have heard of it. Think spices, that's right, the yellow powdery substance. One of the amazing components of Curcumin is the antioxidant effect. Research has shown a significant decrease in mean plasma glucose with curcumin intake (Aziz et al., 2012). The other positive correlations with curcumin are increased HO expression. Increased HO expression leads to increased insulin release and better glucose metabolism as well as significant reductions in LDL cholesterol, triglycerides, and total cholesterol.
OMG Results with Omega-3 Fatty Acids
Neuropathy is the most prevalent symptom when it comes to diabetes. Over half that are diagnosed with diabetes are also diagnosed with neuropathy. The nerve damage happens when the small fiber in the nerves is damaged and eventually affects the large fiber, leading to dysfunction. As the damage occurs, the nerve becomes shorter and less efficient. The damage to the small fiber can be caused by a multitude of health issues, one of which is diabetes (Hovaguimian & Gibbons, 2012). This can almost always be blamed by hyperglycemia. To measure the size of the damage, a corneal nerve fiber length (CNFL) test can be conducted to confirm damage that could lead to neuropathy. The shorter the nerve, the more damage that has occurred.
How can we work to prevent or reverse this damage? Omega-3 fatty acids can be beneficial in preventing small fiber damage from escalating to large fiber dysfunction and even reversing the damage. Omega-3 fatty acids consist of three sources EPA, DHA, and DPA. A study used 750 mg EPA, 560 mg DHA, and 1,020 mg DHA, and found that the CNFL was increased significantly by 29%. Basically, the nerves were repaired, grew, and worked more efficiently (Lewis et al., 2017). In type 1 diabetes the body has dysmetabolism of fatty acids. Research has shown a specific decrease in DHA with type 1. DHA is an essential source of omega-3 fatty acids and has been shown to support nerve growth and aiding in the prevention of neuropathy. Omega-3 fatty acids are also known to decrease inflammation.
Intervene with Berberine
We know that type 1 diabetes involves the destruction of ß cells in the pancreas that produce insulin. T cells are a tool the immune system uses for attacking unknown substances in the body and killing them. The T cells also produce inflammatory responses that are known to be involved with the development of diabetes. Specifically, with diabetes, the islets located in the pancreas are extremely inflamed leading to dysfunction. The supplement, Berberine, is known to aid in the treatment of type 1 diabetes.
Berberine is a substance found in plants. It is a yellow substance similar in color to turmeric. Research shows that berberine significantly reduces inflammatory responses (Cui et al., 2009). Inflammation can cause a fluctuation in blood sugars and cause additional insulin resistance. Inflammation is also known to worsen infections and increase mitochondrial dysfunction, specifically, oxidative stress (Tsalamandris et al., 2019). Remember oxidative stress? Think about the bubble analogy. We want to pop one bubble at a time rather than hundreds. I take berberine and find it to help control my blood sugars with fewer fluctuations. Other effects of berberine include lowering LDL- the bad cholesterol, raising HDL -- the good cholesterol, and reducing triglyceride levels. This is beneficial to everyone, especially those of us that have type 1 diabetes.
Make a Change to Your Routine with Benfotiamine
In type 1 diabetes the insulin signaling pathway does not function properly, leading to hyperglycemia. As we know, hyperglycemia can cause oxidative stress, and can also cause the GAPDH system to deactivate. GAPDH is known to metabolize energy and produce energy for the body to use. By deactivating GADPH system substances called metabolites are released and can cause hyperglycemic damage. Two specific metabolites include glyceraldehyde-3-phosphate and fructose-6-phosphate. (Oh. Et al., 2009). For these metabolites to be metabolized or broken down we need an enzyme known as thiamine-dependent transketolase (TK) to produce them. TK has been shown to be below normal in the diabetic population. So, what can we do to have enough TK to make sure this process is functioning correctly?
Benfotiamine is a derivative of thiamine- vitamin B1. Benfotiamine is more bioavailable than thiamin. Meaning, it is used more efficiently by the body. Research shows that benfotiamine can increase glucose metabolism and insulin synthesis within the cell and help create more TK, thus bringing blood sugars down into a normal range and preventing further complications. Benfotiamine is also known to decrease oxidative stress by blocking three separate pathways that can lead to hyperglycemic damage. (Ratan-NM, M. 2019). There it is again oxidative stress! Blocking the pathways prevents other complications such as nephropathy -- kidney damage and retinopathy -- eye damage.
Disaster Relief Strategies
We talked about how supplements can help decrease oxidative stress, decrease inflammation, and decrease blood sugar fluctuations. We also talked about 5 supplements that can help you control your diabetes; however, I also want to stress the importance of:
- Seeing an endocrinologist regularly
- Stress management
- Healthy sleep practices
- Exercising
- Following a meal plan that will help you best control your diabetes
These supplements are meant to help you, not treat diabetes. Talk to your doctor before trying these supplements. Remember to try your hardest to take control of your diabetes: follow your normal routine, have grace for hard days, and do not let diabetes control you.
References
Abdel, Aziz, M. T., El-Asmar, M. F., El-lrashy, I.N, Rezq, A. M., Al-Malki, A.L., Wassef, M. A., … Morsi, H.M. (2012). Effect of novel water soluble curcumin derivative on experimental type-1 diabetes (short term study). Diabetology and Metabolic Syndrome, 4(1), 1-10. https://doi.org/10.1186/1758-5996-4-30.
Bradley, R. (2007). CoQ10 diabetes information. Retrieved from https://diabetesaction.org/article-coq10.
Cui, G., Qin, X., Zhang, Y., Gong, Z., Ge, B., & Zang, Y.Q. (2009). Berberine differentially modulates the activities of ERK, p38 MAPK, and JNK to suppress Th17 and Th1 T cell differentiation in type 1 diabetic mice. Journal of Biological Chemistry, 284(41), 28420-28429. https://doi.org/10.1074/jbc.M109.012674.
Hovaguimian, A., & Gibbons, C. H. (2012). Nihms271913. 15(3), 193-200. https://doi.org/10.1007/s11916-011-0181-7.Diagnosis.
Lewis, E. J. H., Perkins, B.A., Lovblom, L. E., Bazinet, R. P., Wolever, T.M.S., & Bril, V. (2017). Effect of omega-3 supplementation on neuropathy in type 1 diabetes. Neurology, 88(24), 2294-2301. https://doi.org/10.1212/WNL.0000000000004033.
Montano, S. J., Grunler, J., Nair, D., Takle, M., Fernandes, A.P., Hua, X., … Ungerstedt, J.S. (2015). Glutaredoxin mediated redox effects of coenzyme Q 10 treatment in type 1 and type 2 diabetes patients. BBA Clinical, 4, 14-20. https://doi.org/10.1016/j.bbacli.2015.06.001.
Oh, S. H., Witek, R. P., Bae, S. >, Darwiche, H., Jung, Y., Pi, L., ... Petersen, B. E. (2009). Detection of transketolase in bone marrow-derived insulin producing cells: Benfotiamine enhances insulin synthesis and glucose metabolism. Stem Cells and Development, 18(1), 37-46. https://doi.org/10.1089/scd.2007.0255.
Ratan-NM, M. (2019, May 23). Benfotiamine health benefits and side effects. News Medical Life Sciences. https://www.news-medical.net/health/Benfotiamine-Health-Benefits-and-Si….
Tsalamandris, S., Antonopoulos, A. S., Oikonomou, E., Papamikroulis, G. A., Vogiatzi, G., Papaioannou, S., ... Tousoulis, D. (2019). The role of inflammation in diabetes: Current concepts and future perspectives. European Cardiology Review, 14(1), 50-59. https://doi.org/10.15420/ecr.2018.33.1.
How to Treat Diabetes with the Vegan Diet
Madison Wyatt, Dietetic Intern 2020

Are you thinking about trying the vegan diet? If the vegan diet is new to you, I am here to help! Starting a new way of eating can be scary and exciting all at the same time and I'm here to give you some helpful information to decide if this is the right way of eating for you! If you have diabetes, want to know more about the vegan diet and what the vegan diet can do for you, keep reading!!
What Is the Vegan Diet?
The vegan diet was created officially in 1944 but this way of eating has been around much longer than this, around 2000 years! The vegan diet was created by 6 dairy vegetarians who wanted to eliminate all animal products from their diet. BOOM the vegan diet was created.
The vegan diet is a plant-based diet that excludes all animal products. Yes, this means fish, eggs, dairy, and any other meats! The emphasis is on eating a wide variety of fruits, vegetables, whole grains, legumes, nuts/seeds, and increased fiber.
Per the vegan society, it recommends having fruits and vegetables at least five times per day with a serving size of at least 80 grams. Starchy foods are also recommended, preferably ones rich in fiber, at every meal. Some examples of starchy foods are oats, sweet potatoes, whole-wheat pasta, and brown rice. Plant protein is also important in the diet and should be included at most meals. Some examples of plant proteins are beans, lentils, chickpeas, tofu, and soy alternatives to milk and yogurt such as almond or cashew milk. It is recommended that you consume nuts and seeds, especially those rich in omega-3 fatty acids daily. Calcium-rich foods are also recommended to be consumed ("Vegan Diet - Foods You Can and Cannot Eat, Benefits and Risks," n.d.)
Benefits of the Vegan Diet
The vegan diet has a wide variety of health benefits including improving blood glucose, lowering LDL cholesterol, improving blood pressure, decreasing the risk for cardiovascular disease (CVD), weight loss, overall health, cancer risk, and kidney function. With uncontrolled diabetes, many of these disease complications can occur. The vegan diet is focused on plant foods so this opens up the door to have an overall well-balanced diet. Many people do not consume enough fruits and vegetables, which drastically increases by changing to a vegan diet. Also, according to the Vegan Society, if there was a global movement to changing to a vegan diet it could avert 8.1 million premature deaths ("Statistics", n.d.). Could you imagine??
The vegan diet can be rich in fiber if you do it right. Increasing the amount of fiber by consuming fruits such as berries, fresh vegetables, and whole grains can be beneficial. Fiber helps control blood sugars by being digested slower allowing the blood sugars to stay stable. One study looked at 2 diets, one with moderate fiber and one with high fiber, and how it affected glycemic control in type 2 diabetes. The results showed that higher fiber intake resulted in lower blood sugars and blood sugar stability! It was also found that a high fiber diet had beneficial effects on overall cholesterol and reducing bad cholesterol (LDL) (Chandalia et al., 2000).
Benefits of the Vegan Diet with Diabetes
The vegan diet is a trending diet and it is starting to get recognized in correlation to diabetes. Things that it can help with are improving glycemic control (blood sugars), improving the body's response to insulin, improving LDL cholesterol, and reducing the risk of developing CVD, which is commonly developed with diabetes.
Researchers placed people with diabetes on a low-fat vegan diet and compared them to people eating the diet recommended by the American Diabetes Association (standard diabetes diet). After 22 weeks, people on the low-fat vegan diet had slightly better blood sugar control and as an added benefit, they lost more weight compared to the standard diabetes diet. What was really incredible is that 43% of the participants in the vegan diet group were able to reduce their diabetes medications (Barnard et al., 2006).
This next study was similar in design to the previous study. In the study, researchers compared participants with diabetes consuming an American Diabetes Association diet (conventional diabetes diet) or a low-fat vegan diet. In 74 weeks' results showed that the low-fat vegan diet group had slightly greater weight loss, better hemoglobin A1c levels, and significant improvements in bad cholesterol levels (LDL) (Barnard et al., 2009). The ADA diet is standard as many of you may know and to see that the vegan diet had more improvements means there is another tool that we can use to improve diabetes control.
Insulin resistance is one of the main causes of type 2 diabetes. As we have learned, blood sugar control was seen with the vegan diet but what about insulin resistance? Insulin resistance can also be improved! Researchers looked at a vegan diet compared to an omnivore diet to see if it helped with insulin resistance. Results showed that compared to omnivores, vegans had lower blood pressure and less consumption of harmful fats. It also showed that by consuming a vegan diet, participants became more sensitive to insulin allowing blood sugar to improve (Goff, Bell, So, Dornhorst, & Frost, 2005).
A Vegan Diet Helps Reduce Risk Factors Associated with Diabetes
When diabetes is uncontrolled, there are many risk factors that can come along with it. One of the biggest risk factors is CVD. CVD is the number one cause of death in the United States! CVD is commonly linked with high levels of bad cholesterol, LDL, which we have learned from the previous studies can be decreased with a vegan diet.
More studies have also been linked to showing that there is decreased risk of CVD with the vegan diet. Researchers looked at a low carbohydrate vegan diet compared to a high carbohydrate lacto-ovo vegetarian diet. People on the vegan diet had lower levels of cholesterol, LDL-cholesterol and triglycerides, and improved levels of HDL-cholesterol (the good cholesterol) (Jenkins et al., 2014).
Researchers were also interested in looking at using a vegan diet to decrease the risk of developing CVD and the chance of dying from CVD. Researchers looked at 4 diets ranging from a healthful plant-based diet (full vegan diet) to high consumption of animal products. Over the 20-year period, it showed that participants who consumed a diet rich in plants had a 19% reduced risk of developing CVD or dying from CVD compared to participants who consumed animal products (Kim et al., 2019).
It is amazing what consuming more plants can do to our bodies! As we have learned, the vegan diet is highly correlated with decreasing complications with diabetes and risks associated with diabetes such as CVD. It's a two in one deal!
Common Nutrients to Keep an Eye On
One of the main nutrients we have to watch out for with the vegan diet is Vitamin B12. Vitamin B12 can only be found in animal-based products. It is recommended that people who start a vegan diet consume a vitamin B12 supplement due to the lack of consumption in the diet. Vitamin B12 plays a vital role in the body so a supplement is necessary ("Nutrition overview", n.d.). Other common nutrients of concern are protein, calcium, omega 3 fatty acids, iron, and zinc. These should be monitored are naturally included in a well planned vegan diet ("Nutrition overview", n.d.).
Here are some examples of food sources high in the nutrients of concern:
Protein examples
• Nuts
• Soy
• Beans
• Quinoa
Calcium examples
• Soy milk
• Almond milk
• Cashew milk
• bFortified orange juice
• Broccoli
• Kale
Omega 3 fatty acids examples
• Nuts
• Seeds
• Flaxseeds
• Olive oil
• Plant based supplements
Iron examples
• Tofu
• Soy nuts
• Spinach
• Fortified cereals
• Peanut butter
It is important to monitor these lab values with your doctor and see if an intervention needs to be put in place. The vegan diet is a healthy and safe way of eating despite possibilities of nutrient deficiencies ("Nutrition overview", n.d.).
Vegan Diet Menu I Found and Pinterest
Now that we have learned about all the benefits of why the vegan diet can help control diabetes, I wanted to provide a link to a sample menu that I found on Healthline! Another great source for finding vegan recipes is Pinterest. One of my favorite ones that I have personally made is vegan pesto hummus ?
Give the Vegan Diet a Try!
The vegan diet can help control blood sugars and improve CVD risk (a number one risk factor in people who have diabetes). The vegan diet and how it affects the body is going to be different for each individual. The research has shown that it can be beneficial in diabetes and is worth experimenting with. It is important to be aware of possible nutrient deficiencies and plan your meals/supplements accordingly.
References
Barnard, N. D., Cohen, J., Jenkins, D. J. A., Turner-McGrievy, G., Gloede, L., Jaster, B., … Talpers, S. (2006). A low-fat vegan diet improves glycemic control and cardiovascular risk factors in a randomized clinical trial in individuals with type 2 diabetes. Diabetes Care, 29(8), 1777-1783. https://doi.org/10.2337/dc06-0606
Barnard, N. D., Cohen, J., Jenkins, D. J., Turner-McGrievy, G., Gloede, L., Green, A., & Ferdowsian, H. (2009). A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: a randomized, controlled, 74-wk clinical trial. The American Journal of Clinical Nutrition, 89(5), 1588S-1596S. https://doi.org/10.3945/ajcn.2009.26736H
Chandalia, M., Garg, A., Lutjohann, D., von Bergmann, K., Grundy, S. M., & Brinkley, L. J. (2000). Beneficial effects of high dietary fiber intake in patients with type 2 diabetes mellitus. New England Journal of Medicine, 342(19), 1392-1398. https://doi.org/10.1056/NEJM200005113421903
Goff, L. M., Bell, J. D., So, P. W., Dornhorst, A., & Frost, G. S. (2005). Veganism and its relationship with insulin resistance and intramyocellular lipid. European Journal of Clinical Nutrition, 59(2), 291-298. https://doi.org/10.1038/sj.ejcn.1602076
Jenkins, D. J. A., Wong, J. M. W., Kendall, C. W. C., Esfahani, A., Ng, V. W. Y., Leong, T. C. K., … Singer, W. (2014). Effect of a 6-month vegan low-carbohydrate ('Eco-Atkins') diet on cardiovascular risk factors and body weight in hyperlipidaemic adults: A randomized controlled trial. BMJ Open, 4(2), e003505. https://doi.org/10.1136/bmjopen-2013-003505
Kim, H., Caulfield, L. E., Garcia-Larsen, V., Steffen, L. M., Coresh, J., & Rebholz, C. M. (2019). Plant-based diets are associated with a lower risk of incident cardiovascular disease, cardiovascular disease mortality, and all-cause mortality in a general population of middle-aged adults. Journal of the American Heart Association, 8(16), e012865. https://doi.org/10.1161/JAHA.119.012865
Nutrition overview. (n.d.). Retrieved from https://www.vegansociety.com/resources/nutrition-and-health/nutrition-overview-and-health/nutrition-overview
Statistics. (n.d.). Retrieved from https://www.vegansociety.com/news/media/statistics
Vegan Diet - Foods You Can and Cannot Eat, Benefits and Risks. (n.d.). Retrieved April 18, 2020, from https://www.webmd.com/diet/vegan-diet-overview#2-5
Is Diabetes Making You Lose Your Mind? A Look into the Diabetes + Alzheimer's Connection
Brooke Dunnigan, Dietetic Intern 2019

Have you ever wondered why so many elderly people have Alzheimer's Disease? Maybe you've experienced the heartache of a grandparent forgetting who their spouse and family are, or what they were doing mid-task. Watching someone affected by this disease is heartbreaking and life-altering. In the search for the why, researchers have directed us to the diabetes epidemic contributing to the rise in Alzheimer's Disease. Alzheimer's has been deemed the term Type 3 Diabetes… Ever thought the two could be related? This blood sugar-brain relationship is a hot topic in research and has uncovered a lot of valuable information in the process. Keep reading to learn more on the connection between Diabetes and Alzheimer's disease!
The 411 on Alzheimer's Disease and Diabetes
Before we jump into it, let's talk about the basics.
Alzheimer's Disease
Alzheimer's disease (AD) is a form of dementia that is characterized by memory loss and declining cognitive function and has the ability to change personalities and reduce quality of life. AD makes up between 60 and 80% of dementia cases. AD does not just happen from growing old, though age is a major risk factor. In fact, it plagues close to 200,000 people under 65 in the US. This disease doesn't simply appear, the brain begins to suffer from physiological changes long before symptoms are noticed. The two main changes to the brain are:
1. Beta-amyloid plaques -- deposits of protein particles in the space between nerve cells, blocking the communication which occurs for memory and cognitive function
2. Tangles -- they are what they sound like, fibers that become entangled from a protein called tau ("What is Alzheimer's?" n.d.)
Loss of neurons and synapses (the brain cells and communication pathways), oxidative stress, mitochondrial impairment, slowed neural communication, hormone dysregulation, and irregular cell cycles have been examined in the brains of AD patients (Kandimalla, Thirumala, & Reddy, 2017).
Diabetes
Diabetes is a disease characterized by elevated blood glucose (blood sugar), known as hyperglycemia. Other factors that contribute to diabetes include insulin resistance and poor production of insulin. When we eat something with sugar or carbohydrates, our blood sugar rises. This is normal! The differing factor between a person with diabetes and a person without diabetes is their ability to get their blood sugar back down to normal levels. Insulin is the key player that moves blood sugar into the cells to be used for energy. In type 2 diabetes, insulin resistance means insulin has become less sensitive to this process. The insulin is then circulating in the bloodstream in high amounts (hyperinsulinemia), not doing its job and contributing to inflammation in the body. This can cause a buildup of insulin and glucose in the blood. In someone with type 1 diabetes, they no longer have the ability to produce insulin at all, so they require the administration of insulin in order to regulate blood sugar. For the sake of simplicity, I will not differentiate the types of diabetes for this article; know that I'm referring to both. The longer someone lives in a hyperglycemic state, the more damage it does to the blood vessel lining which can contribute to heart disease, weight gain, retinopathy and nephropathy, kidney disease, and poor cognition (Kharroubi, 2015).
The Blood Sugar-Brain Connection
We tend to think of the brain solely as the control center, telling the rest of the body what to do. In part, this is true, but there's more to the story. In fact, the way we treat the rest of our body has a major impact on our brain's ability to grow, change, and continue developing; this is called neuroplasticity. When we think about it that way, diabetes affecting the brain doesn't seem too far out of left field, right?
What does the research say?
- Older populations with prediabetes and diabetes are at higher risk for cognitive dysfunction. More so than the presence of diabetes, it was poor control of diabetes that led to this association. This connection was characterized by a higher Hemoglobin A1C (HbA1C), which is a measurement of average blood sugar over the past three months. Living in a state of chronically high blood sugar will raise that person's HbA1C and contribute to the risk of cognitive dysfunction. This study also indicated that 1/3 of the patients had symptoms of depression, which has the potential to hinder someone's ability to prioritize diabetes self-management. This can be a dangerously vicious cycle when depression inhibits someone from living out daily tasks such as administering diabetes medication, which can lead to higher blood sugar, thus leading to further memory loss (Munshi, 2006).
- Hyperinsulinemia caused by insulin resistance increases the risk for diabetes 5-fold, but this risk can be lowered by diet and lifestyle modifications (we'll talk about how later). The memory center of the brain is called the hippocampus and it is a hub for insulin receptors. As insulin rises over long periods of time, so does the presence of ß-amyloid plaques, which is a major indicator of AD. This study looked at the middle-aged population around 55 years-old who did not have diabetes. Therefore, even in the absence of diabetes, insulin resistance can still be present and contribute to the buildup of ß-amyloid plaques and contribute to early-onset AD (Young, Mainous, & Carnemolla, 2006).
- Cardiovascular risk factors seen in those with a higher body mass index (BMI) showed a significantly greater presence of ß-amyloid plaques. The population was measured in their "midlife" and again 20 years later. Those with a higher BMI at first measurement proved to have more ß-amyloid plaques in later-life (Gottesman et al., 2017).
- It's safe to say there's sufficient evidence to support the Diabetes-Alzheimer's connection. Let's dive a little deeper into what is causing this connection now that we know hyperglycemia and insulin resistance play star roles in these diseases.
The Culprit: Blood Sugar Dysregulation
We have a guardrail protecting our brain called the blood-brain barrier. Its role is to protect the brain from foreign substances, toxins, and infections that might try to enter via the bloodstream. Insulin, on the other hand, is treated like the VIP molecule in the brain. It passes through the blood-brain barrier with ease and is welcomed by the brain cells (neurons, microglia, and astrocytes). These brain cells have receptors that bind to the insulin circulating in the bloodstream so they can carry out the tasks of:
- Cell growth and reproduction
- Neuroprotection (brain protection against toxins, oxidative stress, and cell death)
- Neuromodulation of hormones and cellular processes of neurotransmitters
- Cognitive and memory function
When insulin resistance gets worse, the brain cells have a more difficult time recognizing the insulin molecules passing through the bloodstream. High amounts of insulin and sugar in the blood lead to brain tissue damage and the brain is unable to carry out the functions needed for brain health.
Obesity paired with insulin resistance is pro-inflammatory in the body, especially in the brain. When large amounts of inflammatory markers such as TNF-a and Interleukin-6 (IL-6) circulate in the brain, they limit the hippocampus' neuroplasticity. This means the part of the brain that is responsible for memory, learning, and emotion, loses its function and more beta-amyloid plaques form (Blázquez, Velázquez, Hurtado-Carneiro, & Ruiz-Albusac, 2014).
Insulin resistance and inflammation in the brain is not a favorable combination. The brain loses the ability to make sound decisions, contain short-term and long-term memories, and modulate mood which can result in depression and anxiety.
What are we supposed to do now?
Protect the Brain with Glucose Regulation
I've mentioned "diet and lifestyle modifications" but what exactly does that mean? "Diet" is a difficult topic, I know. Unfortunately, there is "no one-size fits all" diet, but I will give you an idea of foods to fill up on and foods to steer clear of. And when I say "diet" I don't mean yoyo dieting from one fad to another. Many of us are guilty of it. By "diet" I mean the food you put in your mouth 90% of the time. Physical activity is what I'm referring to when I say "lifestyle." Are you active or inactive? Again, unfortunately, there's no "magic pill" that gives you the benefit of exercise.
Diet
It's important to analyze where you stand in terms of what you eat. Do you tend to order takeout, pick something up in the drive-thru, cook for yourself, binge eat on junk food, or skip meals altogether?
The Standard American Diet (SAD) consists of highly processed foods and refined carbohydrates, not at all what our ancestors ate. These types of foods make it difficult to control blood sugar. While it might taste good at the moment, within an hour you're left hungry and wanting more (due to changes in insulin and blood sugar levels). On top of that, it has been shown to be pro-inflammatory in the brain, increases oxidative stress, and promotes insulin resistance (Berland et al., 2001). Does all of this sound familiar? Sounds like a recipe for diabetes and AD to me!
So, what should you eat?
Let's get back to our roots and eat like our ancestors! Before processed food hit the shelves in the grocery stores people were eating a variety of fruits, vegetables, meat, beans, whole grains, and eggs. Eating a variety of whole foods limits the amount of processed wheat/cereal grains, refined fats and sugars, alcohol, sodas, and added salt. In a study observing people with type 2 diabetes, following this eating pattern over three months significantly lowered their HbA1C, triglycerides, diastolic blood pressure, weight, BMI, and waist circumference. Simultaneously, it raised the anti-inflammatory HDL levels (our "good fat"). These participants also experienced an improvement in fasting blood glucose and insulin levels (Klonoff, 2009). Knowing what we discussed in this article, do you think seeing improvement in these blood measurements would be beneficial to the brain? Yes! Essentially what happened was inflammation, obesity and cardiovascular risks dropped, while insulin sensitivity improved. The cells were able to get the blood sugar they needed quicker!
Now, please don't read this and think "there's no way I can cut out ice cream or french fries!" Start by focusing on building your plate in a way that contains whole-foods, not packaged and processed foods. What you eat 90% of the time is what you should really be aware of. Ice cream after lunch and dinner would mean you're eating it about 66% of the time. So the next step could be working to lower that to 33%, then maybe 15%? Allow ice cream to truly be a special treat, not a daily habit. Becoming aware of the food we put in our mouth allows us to be mindful and think twice about what we're feeding our brain and body.
Exercise
I think it's safe to say that most people know exercise is "good for us," but knowing why really makes a difference in our execution. Sedentary lifestyles have become all too common as technology and Netflix have taken over the world. Okay maybe not in an apocalyptic way, but technology is everywhere you turn your head. This behavior has been connected to blood sugar dysregulation (the culprit for brain inflammation and cognitive dysfunction) and an overall greater risk of death (Wheeler et al., 2017). Partaking in daily exercise at a moderate-intensity can improve brain glucose metabolism and provide neuroprotective benefits (Dougherty et al., 2017). Diabetic or not, exercise improves insulin sensitivity and can lead to a healthier brain and healthier you.
References
Berland, G. K., Elliott, M. N., Morales, L. S., Algazy, J. I., Kravitz, R. L., Broder, M. S., … McGlynn, E. A. (2001). Effects of short-term Western diet on cerebral oxidative stress and diabetes related factors in APP x PS1 knock-in mice. Jama, 285(20), 2612-2621. https://doi.org/10.3899/jrheum.121180.Response
Blázquez, E., Velázquez, E., Hurtado-Carneiro, V., & Ruiz-Albusac, J. M. (2014). Insulin in the brain: Its pathophysiological implications for states related with central insulin resistance, type 2 diabetes and alzheimer's disease. Frontiers in Endocrinology, 5(OCT), 1-21. https://doi.org/10.3389/fendo.2014.00161
Dougherty, R. J., Schultz, S. A., Kirby, T. K., Boots, E. A., Oh, J. M., Edwards, D., … Okonkwo, O. C. (2017). Moderate physical activity is associated with cerebral glucose metabolism in adults at risk for alzheimer's disease. Journal of Alzheimer's disease : JAD, 58(4), 1089-1097. doi:10.3233/JAD-161067
Gottesman, R. F., Schneider, A. L. C., Zhou, Y., Coresh, J., Green, E., Gupta, N., … Mosley, T. H. (2017). Association between midlife vascular risk factors and estimated brain amyloid deposition. JAMA - Journal of the American Medical Association, 317(14), 1443-1450. https://doi.org/10.1001/jama.2017.3090
Kandimalla, R., Thirumala, V., & Reddy, P. H. (2017). Is Alzheimer's disease a Type 3 Diabetes? A critical appraisal. Biochimica et Biophysica Acta - Molecular Basis of Disease, 1863(5), 1078-1089. https://doi.org/10.1016/j.bbadis.2016.08.018
Kharroubi, A. T. (2015). Diabetes mellitus: The epidemic of the century. World Journal of Diabetes, 6(6), 850. https://doi.org/10.4239/wjd.v6.i6.850
Klonoff, D. C. (2009). The beneficial effects of a paleolithic diet on type 2 diabetes and other risk factors for cardiovascular disease. Journal of Diabetes Science and Technology, 3(6), 1229-1232. https://doi.org/10.1177/193229680900300601
Munshi, M., Grande, L., Hayes, M., Ayres, D., Suhl, E., Capelson, R., … Katie Weinger, E. (2006). Cognitive dysfunction is associated with poor diabetes control in older adults. Diabetes Care, 29(8), 1794-1799. https://doi.org/10.2337/dc06-0506
What Is Alzheimer's? (n.d.). Alzheimer's Association. Retrieved May 6, 2019, from https://www.alz.org/alzheimers-dementia/what-is-alzheimers
Wheeler, M. J., Dempsey, P. C., Grace, M. S., Ellis, K. A., Gardiner, P. A., Green, D. J., & Dunstan, D. W. (2017). Sedentary behavior as a risk factor for cognitive decline? A focus on the influence of glycemic control in brain health. Alzheimer's & dementia (New York, N. Y.), 3(3), 291-300. doi:10.1016/j.trci.2017.04.001
Young, S. E., Mainous, A. G., & Carnemolla, M. (2006). Hyperinsulinemia and cognitive decline in a middle-aged cohort. Diabetes Care, 29(12), 2688-2693. https://doi.org/10.2337/dc06-0915
Mushrooms: A Plant-Powered Source of Vitamin D?
Pressley Bailey, Dietetic Intern 2021

At the end of last year, I was on an open road listening to a podcast episode of Lost in the Supermarket by Phil Lempert, titled “Mushrooms: Healthy on the Plate, Gentle on the Planet.” In this episode, Phil reported that mushrooms are the only source of vitamin D found in the produce section (Lempert, 2019). How cool is that?! In this relatively short podcast, I was more intrigued by mushrooms than ever before. Hence the motivation for this blog!
A word on vitamin D
Throughout my education I was taught that micronutrient deficiencies are rare in developed countries. It was not until I was exposed to functional nutrition at the graduate level that I learned the opposite is true for many micronutrients. For example, the U.S. has seen a surge in subclinical vitamin D deficiencies within the last decade. In fact, vitamin D was declared a public health concern for both children and adults in the 2015-2020 Dietary Guidelines for Americans (U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2015). Moreover, this concern was maintained in the 2020-2025 guidelines (U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2020). Why might this be you ask? Well, generally speaking we spend most of our time indoors and when we do go outside, we douse ourselves in sunscreen. In addition to this, the standard American diet lacks whole, nutrient-dense foods that are vital to our wellbeing. It is estimated that we get 80% of vitamin D from the sun and 20% from our food, but as these poor habits perpetuate, our vitamin D status declines (Papadimitriou, 2017). While you know vitamin D is imperative for calcium absorption and bone metabolism, optimal levels of vitamin D are also required for immune support, blood sugar control, cancer prevention, a healthy microbiome, cardiovascular health, and neurological function.
There are a few food sources that naturally contain vitamin D, in the form of D3. The foods that do have natural vitamin D are animal-based, such as salmon, herring, sardines, canned tuna, liver, and egg yolks. The recommended dietary allowance (RDA) for vitamin D is set at 600 IU per day for young adults and 800 IU per day for older adults. The RDA is set by the Institute of Medicine and is considered the average daily level of intake sufficient to meet the nutrient requirements of healthy individuals. However, with a high prevalence of vitamin D deficiencies and their related all-cause mortality, experts have called public health authorities to increase the RDA (Papadimitriou, 2017).
Lets get back to mushrooms
Lo and behold, mushrooms also contain natural vitamin D! This makes mushrooms all the more exciting as they are the only plant-based source of natural vitamin D! In mushrooms, vitamin D is found mostly in the form of D2, although there is detection of vitamin D3 and D4 in some varieties as well. Remarkably, mushrooms can produce more vitamin D through UV exposure, just like we can. In humans, a precursor to cholesterol is used to convert previtamin D3 to vitamin D3. In mushrooms, something similar to cholesterol, known as ergosterol, is used to convert previtamin D2 to vitamin D2 (Cardwell et al., 2018). One study found that consuming 2000 IUs of vitamin D2 from UV light exposed mushrooms was just as effective as consuming 2000 IUs of vitamin D2 or D3 from an oral supplement at increasing vitamin D levels in the body (Keegan et al., 2013). What an incredible finding! According to The Mushroom Council (n.d.), there is 23.6 mcg (about 945 IU) of vitamin D in 5 UV-exposed white button mushrooms, so to obtain 2000 IUs of vitamin D2 from UV-exposed mushrooms, it takes roughly 5 medium-sized button mushrooms twice a day. This means there is potential for mushrooms, a whole food source, to be used as a manageable, affordable, and more enjoyable way to increase vitamin D consumption.
I was utterly sold on this idea that mushrooms are an excellent source of vitamin D. However, I have since learned that fresh retail mushrooms in U.S. supermarkets are typically not exposed to UV light, and thus, do not provide sufficient amounts of vitamin D to the consumer. For example, 5 medium white button mushrooms without exposure to UV light have about 0.18 mcg of vitamin D (The Mushroom Council, n.d.). This amount is negligible considering our goal for vitamin D is at least 15 mcg per day. In the U.S., mushrooms are grown uniquely in atmospherically controlled growing rooms without windows. Because mushrooms lack chlorophyll, they do not get their nutrients from sunlight but rather from the organic matter in the soil. Although this makes mushroom farming highly sustainable, lack of sunlight impedes their vitamin D producing potential. What a bummer this was to discover.
Am I reading this for nothing?
So now you may be wondering where this leaves you – the consumer? According to Cardwell et al. (2018), higher, more sufficient levels of vitamin D can be found in the following mushrooms:
- Fresh, wild mushrooms such as funnel chanterelles.
- Fresh mushrooms deliberately exposed to sunlight for 15-120 minutes between the hours of 11 a.m. and 3 p.m.
- Fresh mushrooms exposed to controlled UV-B radiation via a fluorescent UV lamp or a pulsed UV lamp.
- Dried mushrooms exposed to UV radiation from lamps (i.e., sun-dried, hot-air, and freeze-dried).
While you may not be out of luck necessarily, these mushrooms might be hard to come by, especially at your local supermarket. Nonetheless, these mushrooms are a good option for those interested in increasing their vitamin D intake through diet. Particularly for those who adhere to a vegan or vegetarian diet where vitamin D-rich foods may otherwise be lacking. Furthermore, vitamin D3 supplements are produced from lanolin, a waxy substance derived from sheep, and would not be ideal for someone who opts for a vegan diet (National Institutes of Health, 2021). Instead, this person could look for a vitamin D2 supplement manufactured from mushrooms.
Perhaps you are an overachiever and want to reap the full benefits that mushrooms have to offer – you can grow your own mushrooms (ensuring that they are exposed to sunlight) or place your store-bought mushrooms out in the sun prior to consumption. To maximize vitamin D production, slice your mushrooms to increase their surface area before placing them in the sun. This may sound too good to be true, but one study demonstrated that vitamin D2 increased by at least 25% of the RDA (150 IU) per 70 g serving, and more than 100% of the RDA (> 600 IU) in most cases after 15 minutes of sun exposure on a clear or partly cloudy day (Philips & Rasor, 2013). Although with this method, there are many variables (e.g., the orientation of the sun, weather conditions, geographic locations, etc.), the vitamin D content in these mushrooms after sun exposure was comparable to the level of vitamin D found in fortified foods (i.e., milk and orange juice). Moreover, the level was further increased with continued exposure to sunlight (Philips & Rasor, 2013). See, there is hope!
Mushrooms are powerful, nonetheless!
Despite lower levels of vitamin D in retail mushrooms, mushrooms still make for great nutrition. They are packed with other essential nutrients like B vitamins, selenium, potassium, zinc, and copper. Mushrooms also contain many bioactive compounds, such as ergothioneine and beta-glucan, that have impressive health benefits. Ergothioneine is a sulfur-containing amino acid that has unique and powerful antioxidant properties. In addition to its general antioxidant and anti-inflammatory effects, ergothioneine may aid in the treatment against diabetes, cardiovascular disease, metabolic syndrome, and non-alcoholic fatty liver disease (Lam-Sidun et al., 2021). Beta-glucan is a water-soluble polysaccharide consisting of glucose units. Beta-glucans are attributed to reducing the risk of cardiovascular disease, diabetes, obesity, and cancer, among other findings (Ciecierska et al., 2019). Lastly, mushrooms are affordable, versatile, and great at enhancing the flavor and texture of food.
With suboptimal levels of vitamin D on the rise, this nutrient should be a priority on our plates. So how can you get more vitamin D in your life? Well… more sun (especially between the hours of 11 AM and 3 PM), less sunscreen (especially those with oxybenzone), consume milk, eggs, wild fish, and liver (you brave soul), and as you have just learned…UV light exposed mushrooms!
References
Cardwell, G., Bornman, J., James, A., & Black, L. (2018). A review of mushrooms as a potential source of dietary vitamin D. Nutrients, 10(10), 1498. https://doi.org/10.3390/nu10101498
Ciecierska, A., Drywień, M., Hamulka, J., & Sadkowski, T. (2019). Nutraceutical functions of beta-glucans in human nutrition. Annals of the National Institute of Hygiene, 70(4), 315–324. https://doi.org/10.32394/rpzh.2019.0082
Keegan, R., Lu, Z., Bogusz, J., Williams, J., & Holick, M. (2013). Photobiology of vitamin D in mushrooms and its bioavailability in humans. Dermato-Endocrinology, 5(1), 165–176. https://doi.org/10.4161/derm.23321
Lam-Sidun, D., Peters, K., & Borradaile, N. (2021). Mushroom-derived medicine? Preclinical studies suggest potential benefits of erothioneine for cardiometabolic health. International Journal of Molecular Sciences, 22(6), 5-11. https://doi.org/10.3390/ijms22063246
Lempert, P. (Host). (2019, April 11). Mushrooms: healthy on the plate, gentle on the planet (No. 5) [Audio podcast episode]. In Lost in the Supermarket. SupermarketGuru. https://podcasts.apple.com/us/podcast/mushrooms-healthy-on-the-plate-ge…
National Institutes of Health. (2021, March 26). Vitamin D. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/#h5
Papadimitriou, D. (2017). The big vitamin D mistake. Journal of Preventive Medicine and Public Health, 50(4), 278–281. https://doi.org/10.3961/jpmph.16.111
Philips, K., & Rasor, A. (2013). A nutritionally meaningful increase in vitamin D in retail mushrooms is attainable by exposure to sunlight prior to consumption. Journal of Nutrition & Food Sciences, 3(6), 1-8. https://doi.org/10.4172/2155-9600.1000236
The Mushroom Council. (n.d.). White button. https://www.mushroomcouncil.com/varieties/white-button/
U.S. Department of Health and Human Services and U.S. Department of Agriculture. (2015). Dietary Guidelines for Americans. https://health.gov/sites/default/files/2019-09/2015-2020_Dietary_Guidel…
U.S. Department of Health and Human Services and U.S. Department of Agriculture. (2020). Dietary Guidelines for Americans. https://www.dietaryguidelines.gov/sites/default/files/2021-03/Dietary_G…
Elderberry: Nature's Relief for Cold and Flu Symptoms?
Kelsey Haschke, Dietetic Intern 2019

Nasal congestion, coughing, headaches, aching muscles, and fever; you know what that means! Either the flu or a cold is "knocking at your door". Colds and flu are not fun to experience. If you are looking for a different and more natural way of treating your cold and flu symptoms, then keep reading to answer the question "Elderberry: Nature's Relief to Cold and Flu Symptoms?"
History of Elderberry Use
The elderberry plant's official name is Sambucus. As with all plants, there are several different types of elderberry including (Brobst, 2013):
- Sambucus canadensis: American Elderberry
- Sambucus cerulea: Blue Elderberry
- Sambucus simpsonii: Florida Elder
- Sambucus velutina: Velvet Elder
- Sambucus nigra: European Elder/Black Elderberry
- Sambucus ebulus: Dwarf Elder
- Sambucus melanocarpa: Blackberry Elder
Elderberry plants have been used throughout history for various purposes. These include dyes, medicine, baskets, arrow shafts, and musical instruments. Elderberry usage has even dated back to the time of Hippocrates! Hippocrates called the elderberry his "medicine chest" (Krawitz et al, 2011). The American Botanical Council states the main use for elderberry throughout history has been the treatment of the flu and colds (American Botanical Council, 2004).
Warning: Don't Consume Raw Elderberry
It should be mentioned that it is dangerous to consume raw red elderberries due to cyanide containing compounds. Researchers and medical professionals advise that berries are properly processed and cooked before consumption. It is also advised that pregnant and breastfeeding women do not take elderberry since there is not sufficient research to prove that there are no adverse effects (American Botanical Council, 2004).
So now you're probably wondering what has been researched and what is a safe supplement to use. Let's take a journey of discovery and see what the research says and how to know which supplements are safe.
What Is Research Discovering About Elderberry?
Much research has been conducted on elderberry and its potential to reduce cold and flu symptoms. All of the research seems to be very positive and gives credit to our ancestors for their medicinal use of elderberry for flu and cold symptom reduction. The most common type of elderberry to be researched is Sambucus nigra or the European Elder. Different types of elderberry supplements have been researched as well from berry extracts, lozenges, to syrup!
Our journey for our answer begins with a couple of studies looking at efficacy (how well something can produce a result). One research study looked into how effective oral elderberry extract is in treating Influenza strains A and B. A common elderberry syrup supplement called Sambucol® was used in this study. Half of the participants received Sambucol® and the other half received a placebo. The participants were instructed to take their respective supplements in the amount of 15 mL 4 times per day over 10 days. The study found that the group that received the Sambucol® saw major improvements within 4 days of treatment while the placebo group saw major improvements within 8 days of treatment (Zakay-Rones, Thom, Wollan, & Wadstein, 2004).
The second research article studied the efficacy of an elderberry lozenge on flu symptoms. The elderberry lozenges contained 175 mg of elderberry extract. Half of the participants received the elderberry lozenges and the other half received a placebo lozenge. The participants were told to take the lozenges 4 times per day (1 with each meal and 1 before bedtime). The study found that within 24 and 48 hours of treatment, the elderberry group saw significant reductions in symptoms compared to the placebo group who actually saw worsening of some symptoms (Kong, 2009).
This meta-analysis study looked at 4 research studies and compared each of the studies' findings for similarities. Each study consistently found that all elderberry groups (regardless of the type of supplement) had significantly reduced the severity of symptoms over a placebo group (Hawkins, Baker, Cherry, & Dunne, 2019). It was also noted that flu symptoms were more reduced than cold symptoms, but both were significantly reduced regardless (Hawkins, Baker, Cherry, & Dunne, 2019).
Sambucus nigra or the European Elder or Black Elderberry is the most commonly used plant in elderberry supplements. Now let's take a look at another interesting way to apply elderberry and its symptom-relieving power in another setting: air travel!
Planning on Some Air Travel?
In today's world, air travel is not uncommon. In fact, it is widely used for business or pleasure purposes. Whatever the purpose may be, air travel has found commonplace in today's society. But I'm sure you have heard of people getting cold or flu symptoms while being cooped up on a long flight. Luckily there has been some research over this unpleasant scenario as well! One research article aimed to test how well Sambucus nigra extract could be on cold symptoms and duration for those who were traveling overseas for at least 7 hours. The participants in this study took the extract twice daily for 10 days before their trip until 2 days before their trip, and 3 times daily from 1 day before their trip to 5 days after their trip. This study found that elderberry significantly reduced the duration of a cold by 2 days over a placebo extract and reduced the severity of symptoms as well (Tiralongo et al., 2016). So, for those of you who travel and get cold-like symptoms then there is hope! Be prepared to combat those unpleasant symptoms!
It seems important to take the supplement within the first 24 hours of the onset of symptoms for maximum treatment effects.
Does Elderberry Have Any Other Benefits?
Other research has been done on elderberry as well. Two extra benefits are its possible antibacterial and antiviral effects. It has been proposed that elderberry possesses some antibacterial properties as well as cold and flu symptom reduction abilities. One study aimed to discover just how potent this antibacterial ability was and how effective was an elderberry extract at inhibiting the growth of influenza (flu) A and B viruses. Several types of bacteria associated with upper respiratory symptoms and one sample of the flu A and flu B viruses were subjected to different concentrations of an oral elderberry extract (0%, 5%, 10%, 15%, and 20%). The study found that the elderberry extract at 5% concentrations and above reduced the growth of bacteria and the flu viruses, with the 20% concentration reducing the bacteria to less than 1% growth and significantly reducing the number of virus particles (Krawitz et al., 2011)
Is Elderberry Absorbed Well?
This next study looked at the bioavailability of the antioxidants in an elderberry powder. Bioavailability means how much of a nutrient or compound is available for absorption after digestion. The researchers took some berries from a European Elder plant (Sambucus nigra) and created a powder. The powder was then separated into two halves that were put through two different processes: active and inactive. The study found that after digestion, more than 75% of the antioxidants of the elderberry powder were bioavailable (Zhou, Zhu, Yang, & Zhou, 2016)! This means that over 75% of the antioxidants were absorbable after digestion! It is important to note that this study was designed as an in vitro study, which means that it was done in a test tube.
What Is a Reputable Elderberry Supplement?
Isn't it great that the research shows that elderberry has a great impact on reducing cold and flu symptoms! So now you are probably wondering "what should you do with this information?" There are so many types of elderberry supplements out there that it is very easy to get confused, and very quickly at that. According to Dr. Taz Bhatia, an integrative medicine doctor, there a couple of items to look for on a supplement bottle to ensure that you are getting a quality supplement. These items to look out for include (Bhatia, 2016):
- Is the supplement either USP or NSF certified?
- Are all the ingredients listed?
- Is an expiration date on the container?
- Does the company mention any third-party testing?
Each of these items helps ensure that you, a health-minded individual, receive the highest quality supplement on the market. Having a USP or NSF certification ensures that the manufacturing company is following safe manufacturing practices. It is important to know what is in your supplement. Expiration dates are not something new. Checking for an expiration date ensures consumer health and can give a hint to how old a supplement is or how long it has been sitting on a shelf. Third-party testing ensures once again that the supplement is safely manufactured following safe practices under the USP or NSF guidelines. Third-party testing can also test to see if the ingredients listed in the label are actually what are in the product as well. These items apply to all types of elderberry supplements such as extracts, pills, lozenges, and syrups. Purchasing a high-quality supplement will, in the long run, keep you safe and ensure that you are receiving the treatment you deserve!
Answering the Question: "Elderberry: Nature's Relief to Cold and Flu Symptoms or Outdated Treatment?"
I hope you have learned a natural alternative to treat your cold and flu symptoms. The research that has been presented here shows great promise for elderberry supplementation. It seems that our ancestors had the right idea when they started using elderberry as a medicinal herb for cold and flu symptoms. Follow this link to see a doctor's opinion on elderberry supplementation: https://drlowdog.com/elderberry-for-cold-flu-season/. Be sure and consult your healthcare practitioner on any supplements that you take.
References
American Botanical Council. (2004). The ABC Clinical Guide to Elderberry. Retrieved from http://cms.herbalgram.org/press/files/elderberry-scr.pdf
Bhatia, T. (2016). What makes a good supplement? Retrieved from https://doctortaz.com/what-makes-a-good-supplement/
Brobst, J. (2013). Elderberry: The Herb Society of America's Essential Guide. Retrieved from https://www.herbsociety.org/file_download/inline/a54e481a-e368-4414-af68-2e3d42bc0bec
Centers for Disease Control and Prevention. (2019). 2018-2019 U.S. Flu Season: Preliminary Burden Estimates. Retrieved from https://www.cdc.gov/flu/about/burden/preliminary-in-season-estimates.htm
Hawkins, J., Baker, C., Cherry, L., & Dunne, E. (2019). Black elderberry (Sambucus nigra) supplementation effectively treats upper respiratory symptoms: A meta-analysis of randomized, controlled clinical trials. Complementary Therapies in Medicine, 42, 361-365. https://doi.org/10.1016/j.ctim.2018.12.004
Kong, F.-K. (2009). Pilot Clinical Study on a Proprietary Elderberry Extract: Efficacy in Addressing Influenza Symptoms (Vol. 5). Retrieved from https://pdfs.semanticscholar.org/367d/1c92716b6be462f26dbfe6c223863dc78464.pdf
Krawitz, C., Mraheil, M. A., Stein, M., Imirzalioglu, C., Domann, E., Pleschka, S., & Hain, T. (2011). Inhibitory activity of a standardized elderberry liquid extract against clinically-relevant human respiratory bacterial pathogens and influenza A and B viruses. BMC Complementary and Alternative Medicine, 11(1), 16. https://doi.org/10.1186/1472-6882-11-16
Low Dog, T. (2018). Elderberry for Cold and Flu Season. Retrieved from https://drlowdog.com/elderberry-for-cold-flu-season/
Tiralongo, E., Wee, S., Lea, R., Tiralongo, E., Wee, S. S., & Lea, R. A. (2016). Elderberry supplementation reduces cold duration and symptoms in air-travelers: A randomized, double-blind placebo-controlled clinical trial. Nutrients, 8(4), 182. https://doi.org/10.3390/nu8040182
Zakay-Rones, Z., Thom, E., Wollan, T., & Wadstein, J. (2004). Randomized study of the efficacy and safety of oral elderberry extract in the treatment of influenza A and B virus infections. Journal of International Medical Research, 32(2), 132-140. https://doi.org/10.1177/147323000403200205
Zhou, N., Zhu, W., Yang, F., & Zhou, K. (2016). In vitro gastrointestinal digestion model to monitor the antioxidant properties and bioavailability of phenolic antioxidants from elderberry. Reactive Oxygen Species, 2(6), 421-431. Retrieved from https://aimsci.com/ros/index.php/ros/article/view/59/150
How to Avoid Getting Sick: Food, Move and Soothe
Alexandria Broadbent, Dietetic Intern 2017

Big life changes can take a toll on the body: starting at a new university, a new job, moving to a new city… Sometimes when these changes happen, we don't always remember to take care of ourselves, so a lot of times, we get sick. Let's take a look at three major ways within our control that can help keep our immune system in check so this is less likely to happen! As my mama always says, "it stinks to be sick".
Diet
Diet plays a huge role in the function of the immune system. Here is a summary of a few of the vitamins that contribute greatly and why they are so important. Let's go alphabetically:
- Vitamin A makes sure that the mucosal barriers separating the outside world from our inside world stays strong. These barriers are in the digestive tract, respiratory tract, and even our eyes. Another function of Vitamin A is to produce the appropriate inflammatory response (Maggini et al., 2007). Inflammatory response is the reaction to any negative stimuli in the body. When a mosquito bites us, it gets red and swells. That's the inflammatory response on a small scale. Vitamin A keeps that process in check so the appropriate cells are taking action to clear up the issue ASAP. Vitamin A can be found in liver, eggs, and dairy products. A precursor to Vitamin A, beta-carotene, is mostly found in orange/red vegetables: carrots, tomato, sweet potato, and butternut squash, just to name a few.
- Vitamin B6 breaks down dietary proteins. These proteins break down into amino acids which are used for building antibodies and cytokines (Maggini et al., 2007). Antibodies and cytokines are created for the sole purpose of defending the body from foreign invaders! B6 is found in high amounts in fish, meats, and is in some produce like bananas, spinach, and sweet potato.
- Vitamin C seems to be a popular vitamin when we get sick. Does it really help us recover? That's a good question! Well, research has shown that Vitamin C intakes had no effect on prevention of getting sick. There is hope, though. Vitamin C did have a significant effect on decreasing the duration of common cold symptoms. There does seem to be one caveat. Athletes who perform in extreme weather have a 50% reduced chance of getting sick with consistent intake of Vitamin C (Hemila & Chalker, 2013). That is some powerful stuff! But it definitely won't keep you from getting sick unless you are an extreme athlete. And remember, don't wait until you're sick to get your C-stores up! You can find vitamin C in citrus, bell peppers, kale, and many fruits.
- On to Vitamin D. It has been shown to support antimicrobials in the respiratory system lining and increases activity in the body's defensive cells. Vitamin D is special because it has a protective factor that can influence the occurrence autoimmunity (Maggini et al., 2007). Getting enough Vitamin D is quite difficult. One solution that we always have is the sun (for at least 10 hours a day)! Our bodies can convert sunshine into vitamin D. It does take quite a bit of time for this method to happen, and you do have to be careful not to get sunburned! This process is not as reliable in those with darkly pigmented skin or those living in cold regions. Some foods with Vitamin D are fatty fish, fortified beverages like milk and OJ, and egg yolks.
- Vitamin E also plays an important role in immune health. It helps to trigger the white blood cell action when infectious agents enter the body. Vitamin E supplementation can be beneficial to counteract the effects of decreased immune response with age (Bunout et al., 2004). Some sources of Vitamin E are nuts, cooking oils, avocado, spinach, and sweet potato.
I know what you're thinking. It does seem like these vitamins all kind of do the same thing. In the grand scheme of things, that is correct. But in different ways. For example, creating a lymphocyte (defensive white blood cell) is a process. Every vitamin will play a necessary role in each step -- from creating a lymphocyte to activating it into battle. We can't do it without our little vitamin friends working together to keep us safe.
So what is the overall takeaway for diet and immune support? Supplements are okay, but quality is hard to find at an affordable price. It is also difficult to know what to look for when there are so many options out there. Basically what we need to do is eat more fruits and vegetables (like we didn't see that coming). But really, many Americans are lacking in this department. The recommended amount is to reach is 9 servings per day. We also need to eat a wide variety of whole foods. These sources of vitamins and minerals are the most natural and effective way for our bodies to get what they need to keep on ticking. Whole food provides the complimentary nutrients that we need in order to fully absorb these key vitamins (Gershwin et al., 2004). Supplements just can't fake that.
Exercise
We have all been there before: spending most of our time caught up in life, and not putting physical activity at the forefront of our minds. Let's say that one day we finally have some free time and decide to play a game of 2v2 basketball. The next day we are so sore and regret ever doing it! Research shows that acute bouts of exercise like this actually lower the immune system by increasing inflammation (Walsh et al., 2011). However, regular exercise (4-7 days/week) has been shown to improve the immune system. Moderate training a few times a week promotes adaptation of the immune system, improving and increasing the function of immune cells (Fuente et al., 2005). Exercise can be a scary word for some people. Just think of it as moving more! Hitting the gym or running 10 miles isn't for everyone. Walking the dog, playing with your kids at the park, or going for a swim are some (fun) ways to reach a physical activity goal. The main thing is to move.
Stress
No matter what stage of our lives, we are all going to experience some kind of stress-whether it is physical or emotional. Both kinds can take a toll on the body. I experienced this first hand with struggles in my personal life. I was sick for about 6 weeks with an infection, migraines, and acne breakouts. All my terrible symptoms began to resolve once my emotional stress decreased, which happened when everything finally settled down. SO, needless to say, emotions can certainly have an affect on physical health.
Not everyone is affected in the same way by stress. It can depend on the person's genetics, coping mechanism, personality, and social support available (Shapiro et al., 2005). Chronic, or continuous stress, can increase a person's risk for diabetes, asthma, depression, and tumor development (Salleh, 2008). Freaky, huh? This just shows, we all need to take a breather. We usually make time to brush our teeth 2-3x a day, we can certainly set a few minutes aside each day to relax or cope however we do best. Some people say that yoga is the best kind of stress reliever, but it's really just as effective as relaxation alone (Smith et al., 2006). But, please, if you want to knock out two birds with one stone (exercise and stress reduction), go for it!
Temporary stress, however, like first date nervousness, game day anxiety, or giving a speech can be good for us! Instead of putting us in distress, these kinds create eustress. Eustress is what makes us get out of bed in the morning, gives us a competitive edge, or enthusiasm to project across the crowd. Eustress allows us to adapt. Distress holds us back (Salleh, 2008).
Now, as we age, we should expect many changes in our bodies. This includes microscopic changes in our immune system. Our body is not able to produce lymphocytes the way it used to (Linton, et al, 2004). This makes it even more important to strengthen our immunity and take care of ourselves to the best of our abilities, especially as we age.
So get out there and get the right food, move more and soothe your tensions!
References
Bunout, D., Barrera, G., Hirsch, S., Gattas, V., de la Maza, M.P., …, & Munoz, C. (2004). Effects of a nutritional supplement on the immune response and cytokine production in free-living Chilean elderly. Journal of Parenteral Enteral Nutrition, 28: 348 -354.
Fuente, M., Hernanz, A., & Vallejo, M.C. (2005). Forum review: The immune system in the oxidative stress conditions of aging and hypertension: Favorable effects of antioxidants and physical exercise. Antioxidants & Redox Signaling, 7 (9&10): 1356-1366.
Gershwin, M.E., Nestel, P., & Keen, C.L. (2004). Handbook of nutrition and immunity. Totowa, NJ: Humana Press Inc.
Hemila, H., & Chalker, E. (2013). Vitamin C for preventing and treating the common cold (Review). The Cochrane Library, 2013(5): 1- 103.
Linton, P.J., & Dorshkind, K. (2004). Age-related changes in lymphocyte development and function. Nature Immunology, 5:133-139.
Maggini, S., Wintergerst, E.S., Beveridge, S., & Hornig, D.H. (2007). Selected vitamins and trace elements support immune function by strengthening epithelial barriers and cellular humoral immune responses. British Journal of Nutrition, 98(1): S29-S35.
Salleh, M.R. (2008) Life event, stress and illness. The Malaysian Journal of Medical Sciences, 15(4): 9-18.
Shapiro, S.L., Astin, J.A., Bishop, S.R., & Cordova, M. (2005). Mindfulness-based stress reduction for health care professionals: Results from a randomized trial. International Journal of Stress Management, 12(2):164-176.
Smith, C., Hancock, H., Blake-Mortimer, J., & Eckert, K. (2006). A randomized comparative trial of yoga and relaxation to reduce stress and anxiety. Complementary Therapies in Medicine, 15: 77-83.
Walsh, N.P., Gleeson, M., Shephard, R.J., Gleeson, M., Woods, J.A., …, & Simon, P. (2011). Position statement part one: Immune function and exercise. Exercise Immunology Review, 17: 6-63.
Renal Frustration
Michelle McDaniels, Dietetic Intern 2022

Has your nephrologist told you that your kidneys are failing and there’s nothing you can do about it? Are you overwhelmed with the mountain of contradicting information that confronts you as you attempt to do online research? Do you feel like you are on the fast track to dialysis and that you are completely helpless to do anything to change it? Believe it or not, that is a very common complaint for people with chronic kidney disease (CKD). Many people with CKD have a declining glomerular filtration rate (GFR) and they don’t know if they have 3 decades or 3 months before they need to begin thinking about dialysis. The good news is, there are things you can do to slow the progression of CKD, starting with your diet. The bad news is, nutrition is the world’s best-kept secret, so even your nephrologist may not be aware of these evidence-based interventions. There are several things you can do to reduce the burden on your kidneys, starting with diet. This article will focus on a specific diet called the PRAL diet. Additionally, it will link to a few additional interventions below. Before you read on, you may want to refer to my article Understanding ESRD to provide some background information.
How Can Diet Slow Down Kidney Disease?
Have you ever heard of the alkaline diet? It’s been a few years since the craze, but maybe you remember the books, the advertisements, or the grocery store isles exploding with crates of alkaline water. Well, maybe the alkaline diet felt a little gimmicky to some of us, but the idea behind it was to increase alkalinity and reduce acidity to create a better environment in the body and reduce risks of chronic disease. Unfortunately, it didn’t really catch on because many of us know that our body has its own pH regulatory system which is very hard to overcome. So, no matter how many alkaline foods you consume, you will not easily overcome the body’s buffers. However, in a body without a properly functioning pH regulatory system, the alkaline diet concept may actually hold water. This leads us to the topic of the PRAL diet.
Potential Renal Acid Load (PRAL) is a term used to describe the amount of acidity that the metabolism of your food produces for your kidneys. Since one of the jobs of your kidneys is to balance acid load, a reduction in acid load can alleviate the burden that your kidneys face. Here is a list of studies that have shown that following a PRAL diet can reduce the acid load on kidneys and improve CKD outcomes:
- In an analysis of 4,564 Iranian adults, researchers found a link between low GFR and high PRAL (Miriman, 2016).
- Researchers discuss the evidence that alkaline and low-protein vegan diets are better treatments for metabolic acidosis than traditional bicarbonate supplementation (Noce, 2021).
- This three year trial tested a PRAL diet vs bicarbonate supplementation in CKD patients and showed that the PRAL diet was more effective in preserving GFR and decreasing excretion of beneficial hormones (Goraya et al., 2014).
- Researchers discuss the benefits of reduced dietary acid load, including preservation of bone and muscle, preservation of GFR, and prevention of subclinical acidosis (Scialla & Anderson, 2013).
Sold, right? The PRAL diet sounds great! But what exactly is the PRAL diet? Let me explain. PRAL diets focus mainly on the intake of alkalizing fruits and vegetables and avoid animal proteins and grains, which are acidic. You might wonder, aren’t I supposed to stay away from fruits and vegetables? Don’t those have a lot of phosphorus and potassium? Let me dispel that myth for you. Yes, you may need to watch your phosphorus and potassium if those levels are above normal on your labs. However, you will absorb a much higher percentage of the phosphorus and potassium additives from processed foods than the natural forms found in fruits and vegetables (Cases et al., 2019). As a matter of fact, plenty of studies have been done showing that people with CKD can exist on a diet of primarily fruits and vegetables without ever having high potassium or phosphorus. Furthermore, according to Gluba-Brzózka et al. (2017), the National Kidney Foundation recommends a vegetarian diet for patients with CKD. So, a diet high in fruits and vegetables can actually be better for maintaining balanced phosphorus and potassium levels, not worse. Now that that’s out of the way, let’s get back to the PRAL diet. The PRAL diet, again, is going to focus on alkalizing foods, primarily fruits and vegetables. When it comes to the PRAL diet, not all plants are created equal, however. One thing to remember: when it comes to acidity, we are more concerned about the products that are created by the food than the food itself. For example, oranges are acidic when eaten, but become alkaline once they are metabolized by our bodies. Another important thing to note is that alkaline diet does not mean vegan diet. Grains typically produce more acidic compounds in the body than fruits and vegetables, and anyone who has tried a vegan diet knows that grains can often be the star of the show. So, I mentioned avoiding meat and you are probably wondering about that. Unfortunately, any animal product will produce a considerable amount of acidity, with the exception of goat cheese. To give you a better idea, below are 2 lists of acidic and non-acidic foods.
Acidic foods to avoid:
- Most grains (except those listed in the alkaline list)
- Sugar (especially processed)
- Artificial sweeteners except stevia
- Dairy from cows
- Meat and fish
- Beer and soda
- Corn oil, peanuts, walnuts
- Potatoes, beans
- Blackberries, cranberries, prunes
Alkaline foods to focus on:
- Amaranth, millet, wild rice, quinoa
- Maple syrup, raw honey
- Stevia
- Goat milk and cheese
- Soy protein
- Herbal tea, lemon water
- Olive oil, almonds
- Asparagus, cruciferous, green leafy, squash, root vegetables, mushrooms
- Citrus, melon, apple, pear, avocado, blueberries
As you can see, not all fruits and vegetables are alkaline! You can probably see where this can become confusing, but not to worry. The alkalinity varies for each, but as a rule of thumb, fruits and vegetables are almost all more alkalizing than meats and grains. You might be wondering: Can I balance acidic foods by eating more alkaline foods? The answer is yes, sort of. It takes a lot of alkaline fruits and vegetables to balance a steak sandwich. We also know that it is nice to have a few bites of steak or a sprinkle of cheese on occasion, so my recommendation would be to avoid acidic foods for the most part, but don’t feel bad for adding some fetta to your salad on occasion! Just know that the more alkaline foods you consume and the more acidic foods you avoid, the better results you will have. For a better understanding, here is a study that discusses PRAL in further detail and provides a list of alkaline foods: The Alkaline Diet: Is There Evidence That an Alkaline pH Diet Benefits Health? (Scialla et al., 2013).
Low Protein: An Unlikely Benefit?
As I mentioned before, the main focus of the PRAL diet is to reduce acidity. Well, there’s an added benefit of the PRAL diet—it is low in protein. You might be asking, how is this a good thing? Don’t I need protein? The answer is yes, but balance is key. Protein is very hard for the kidneys to filter, and if you have CKD, excess protein can speed up the rate of damage. If you have kidney disease and you aren’t on dialysis, your estimated protein needs are pretty low. If you are on dialysis, your protein needs will be a little higher because some protein is lost during dialysis. It is always best to adjust protein needs under the supervision of a qualified practitioner. Protein is necessary for muscle maintenance as well as a host of important metabolic functions, so getting the right amount is important! One good bit of news is that is entirely possible to consume the amount of protein you need from plant sources. Great sources of plant protein are tofu, beans, peas, nuts and seeds. While these are not the most alkalizing plant foods, they are way less acidic than meat and processed grains. Just remember to balance it out with lots of brightly colored fruits and vegetables!
Supplements
I won’t go too far into supplements in this article, but I would be remiss not to at least mention them. There are a few supplements which have been shown to alleviate some of the metabolic burden on the kidneys, and if you are already consuming a low-protein PRAL diet, these supplements can be a great addition to your regimen.
Keto-Analogue Supplements
Another trick you can use to slow down the progression of CKD is the addition of a keto-analogue supplement. These supplements are of double benefit because they uptake toxins from the blood and allow you to consume even less protein, reducing even more stress on the kidneys. This can be a tricky balance, however, so it is always advised to do this under the care of a qualified healthcare practitioner. To learn in more detail, click here to read my blog Keto-analogue Supplements and VLPD for CKD.
Probiotics
If you’re anything like the rest of us, you’ve heard quite a bit about probiotics by now. The gut microbiome is a fascinating area of research and probiotics have been shown to be useful in mood, digestion, immunity, weight loss, and even skin problems. But did you know there is research that shows that certain forms of probiotics can be beneficial for CKD patients as well? It turns out that the toxins accumulated in the body as a result of CKD don’t only increase your blood levels, they have an impact on your gut microbiome as well! To learn more, click here to read my blog Dysbiosis and CKD.
Wrap it Up
Hopefully this article has served to provide you with a little understanding of what you can do to take the reins on your CKD. Please remember that these lifestyle changes should be done under the supervision of a credentialed healthcare practitioner. It may seem overwhelming, but there is support out there! Visit this link to check out the free CKD Nutrition Support Group. If you are ready to take the plunge, visit this link to schedule a free 30-minute assessment. If this sounds like a lot, don’t worry, you are not alone. Taking it one step at a time makes this process completely doable, and your kidneys will thank you for it!
References
Cases, A., Cigarrán-Guldrís, S., Mas, S., & Gonzalez-Parra, E. (2019). Vegetable-based diets for chronic kidney disease? It Is Time to Reconsider. Nutrients, 11(6), 1263. https://doi.org/10.3390/nu11061263
Goraya, N., Simoni, J., Jo, C. H., & Wesson, D. E. (2014). Treatment of metabolic acidosis in patients with stage 3 chronic kidney disease with fruits and vegetables or oral bicarbonate reduces urine angiotensinogen and preserves glomerular filtration rate. Kidney Iinternational, 86(5), 1031–1038. https://doi.org/10.1038/ki.2014.83
Gluba-Brzózka, A., Franczyk, B., & Rysz, J. (2017). Vegetarian diet in chronic kidney disease-A friend or foe. Nutrients, 9(4), 374. https://doi.org/10.3390/nu9040374
Mirmiran, P., Yuzbashian, E., Bahadoran, Z., Asghari, G., & Azizi, F. (2016). Dietary acid-base load and risk of chronic kidney disease in adults: Tehran lipid and glucose study. Iranian Journal of Kidney Diseases, 10(3), 119–125.
Noce, A., Marrone, G., Wilson Jones, G., Di Lauro, M., Pietroboni Zaitseva, A., Ramadori, L., Celotto, R., Mitterhofer, A. P., & Di Daniele, N. (2021). Nutritional approaches for the management of metabolic acidosis in chronic kidney disease. Nutrients, 13(8), 2534. https://doi.org/10.3390/nu13082534
Schwalfenberg G. K. (2012). The alkaline diet: is there evidence that an alkaline pH diet benefits health?. Journal of Environmental and Public Health, 2012, 727630. https://doi.org/10.1155/2012/727630
Scialla, J. J., & Anderson, C. A. (2013). Dietary acid load: a novel nutritional target in chronic kidney disease?. Advances in Chronic Kidney Disease, 20(2), 141–149. https://doi.org/10.1053/j.ackd.2012.11.001
Verzola, D., Picciotto, D., Saio, M., Aimasso, F., Bruzzone, F., Sukkar, S. G., Massarino, F., Esposito, P., Viazzi, F., & Garibotto, G. (2020). Low protein diets and plant-based low protein diets: do they meet protein requirements of patients with chronic kidney disease?. Nutrients, 13(1), 83. https://doi.org/10.3390/nu13010083
Are Food Dyes Causing My Child to be Hyperactive?
Heidi Paul, Dietetic Intern 2020

The most enduring and controversial issue with attention-deficit/hyperactivity disorder (ADHD) is the possible role of food additives/artificial dyes in the development of the disorder, especially in children.
ADHD Throughout the Years
According to the Centers for Disease Control and Prevention (2020), ADHD is one of the most common neurodevelopmental disorders in children. Millions of US children have been diagnosed with ADHD and diagnoses among children continue to rise every year.

Source: Xu et al., 2018
Although the exact cause of ADHD is unknown, studies have raised concerns regarding the effect of artificial food dyes on child behavior and their role in exacerbating ADHD symptoms. Children are particularly more susceptible to the effects of these dyes since their bodies are still developing and undergoing substantial changes and maturations that are more vulnerable to disruptions (Trasande, Shaffer, & Sathyanarayana, 2018).
Professional opinion on this issue has trended toward skepticism because studies have varied widely in terms of study length, sample size, methodological consistency, and artificial food dyes which varied in amounts and dyes selected (Stevens, Kuczek, Burgess, Hurt, & Arnold, 2011). Thus, further work is needed to better understand the implications of artificial food dye exposure and resolve the uncertainties across the scientific evidence.
What's with the Food Dyes?
The purpose food dyes serve is to add "enjoyment" to our foods by maintaining or improving their appearance. Manufacturers most notably use food dyes because they are cheaper, more stable, and brighter than most natural colorings.
Artificial food dye consists of chemicals used to add color to food and is often added to processed foods, beverages, and condiments. In particular cereals, candy, snacks, vitamins, and many other products designed for children are colored with dyes (Potera, 2010).
Unlike other food additives, dyes are not permitted unless the U.S. Food and Drug Administration (FDA) tests and certifies that each batch meets the legal specifications. The FDA is also responsible for testing the safety of food coloring, along with overseeing all food additives, stabilizers, and preservatives for public consumption. The FDA has given Generally Recognized as Safe (GRAS) status to 9 food colors:
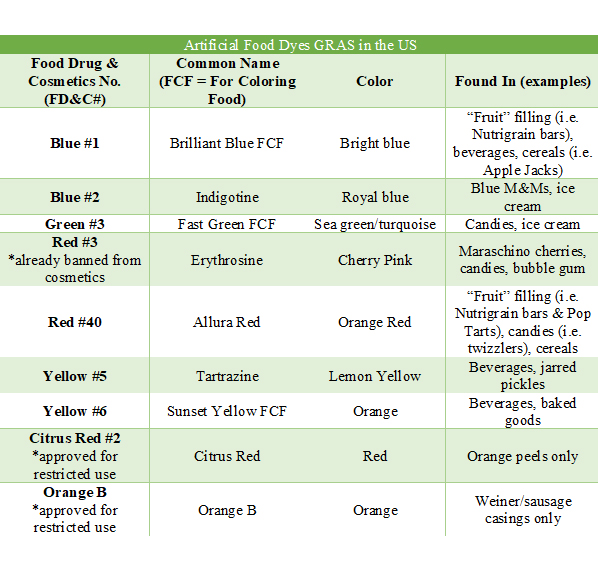
However, many of the nine currently approved dyes have raised public health concerns as they are likely carcinogenic, cause hypersensitivity and behavioral problems, or are inadequately tested (Kobylewski & Jacobson, 2010).
What Researchers Are Saying
There has been a lot of debate on whether or not food dyes can cause hyperactivity and other problematic behaviors observed in children. This topic was first introduced in the 1970s through the work of Benjamin Feingold (Kanarek, 2011). Feingold claimed that some children exhibiting problem behaviors, including hyperactivity and learning disabilities, exhibited noteworthy improvement when following an elimination diet consisting of excluding foods with artificial colors and flavors. Conversely, when children were exposed to foods with artificial colors and flavors, even in small trace amounts, there was a deterioration in their behavior. Based on these clinical observations, Feingold's elimination diet became a more prominent treatment for hyperactivity among the general public. These observations would set the scene for the next 30 + years (Potera, 2010).
In 2012, Arnold, Lofthouse, and Hurt reviewed multiple studies analyzing the effects of artificial food dyes and preservatives on ADHD. They discovered that current research does not necessarily support the view that ADHD is caused by food additives or coloring. On the contrary, research does show that these ingredients can potentially make symptoms worse in those affected by ADHD (Arnold et al., 2012). Dr. Arnold further discussed his team's research findings, stating that it is difficult to understand the true effect of artificial food dyes as many of the published research "lump" artificial food dyes together making it challenging to distinguish which colors may be of more harm. This suggests that additional research designed for determining if artificial dyes have a role in children's behavior is essential (Arnold, 2016).
Additionally, Nigg, Lewis, Edinger, and Falk (2012) reviewed multiple studies and concluded that color additives do affect hyperactive behavior in children, with a small subgroup exhibiting more extreme behavior than others. It was also discovered that a child does not have to have ADHD to have a sensitivity to artificial food colors that result in behavioral or attention problems when these additives are consumed. Concluding that further research is needed because many of the studies only observed small numbers of people or were unable to draw conclusions about the general population. Furthermore, studies have shown removing foods containing artificial dyes via restriction diets may successfully decrease hyperactivity. However, Nigg et al. (2012) claim this is likely due to the removal of processed foods, which are healthier and result in better behavioral outcomes for children with ADHD. Given that such effects have been observed in children, a thorough reassessment of artificial food dyes is warranted to determine their safety (Trasande et al., 2018).
The FDA's Role on This Question: Is Food Coloring Toxic?
The FDA maintains artificial food dyes are safe, yet research has found dyes may contribute to hyperactive behavior in children.
In 2011, the FDA arranged a Food Advisory Committee meeting after the Center for Science in the Public Interest (CSPI) petitioned the FDA to review the evidence on whether or not artificial dyes used to color food contribute to hyperactivity in children (Potera, 2010; CHADD, 2017). Although they admitted that some children are sensitive to food dyes and that this may have an effect on ADHD symptoms, they concluded that there was insufficient evidence that foods with artificial dyes cause hyperactivity in the general population. The FDA also determined that further research is necessary and that a label revealing a possible link between dyes and hyperactivity is unnecessary at this time (Weiss, 2012). Since then, the FDA has decided to allow the use of dyes until harm is more definitively proven.
What Other Countries Are Doing
Many European countries do not allow artificial colors and dyes altogether. Since 2010, the European Union (EU) countries have added a warning label to foods containing synthetic dyes indicating they may increase inattention or hyperactivity.
In 2007, a study in the UK revealed that artificial colors and/or the common preservative sodium benzoate increased hyperactivity in both hyperactive children and non-hyperactive children, suggesting that the dyes are a public health concern (McCann et al., 2007). It was after this study was published, the British government required the food and restaurant industries to eliminate the dyes tested by the end of 2009. And at the beginning of 2010, the EU passed a law that would require a warning label on all foods that contain one or more of the dyes tested (yellow food dyes No. 5 and No. 6, and red dye No. 40). The following warning label states "may have an adverse effect on activity and attention in children" (Weiss, 2012).
What's Being Done About It Here
If you consume orange soda in the US, you're consuming red #40 and yellow #5. But, in the EU, you're drinking pumpkin and carrot extract. Products manufactured by McDonald's, PepsiCo, and other major US multinational companies contain dyes in the US, yet natural or no colorings in the UK (Kobylewski & Jacobson, 2010). The trend is stronger in the EU than in the US, however, some food manufacturers in the US are slowly removing artificial dyes from their products and replacing them with natural alternatives.
Although it is not required for food manufacturers in the US to provide a warning label on foods containing synthetic dyes, many manufacturers are opting for a more natural approach when it comes to their products in food that is marketed to children.
Since the policy changes in the EU were centered heavily on a population study in England, Nigg et al. (2012) suggested that there is an urgent need for an updated, accurately conducted study in the US.
What's Next?
Because there is no definitive answer, companies are permitted to use synthetic additives such as food dyes in their products. The bottom line is that artificial food dyes provide no nutritional benefit, therefore, there is no need for artificial food dyes in your child's diet.
Truthfully, we are a long way from following standards utilized in the EU and banning questionable artificial food colors. However, if you are concerned that food dyes are affecting your child's behavior, then there are safer alternatives for you and your family. Many families have found ways to avoid these ingredients, which are often found in prepackaged foods. As a general rule of thumb, these foods are not usually the healthiest choices available. Look for items identified by "No Artificial Flavors or Colors" label on packages and check labels for added preservatives and unnatural ingredients. Try finding products with natural dyes, such as anthocyanins (grapes), betacyanin (beets), carmine (extracted from crushed cochineal insects), lycopene (tomatoes), annatto (Bixa Orellana tree), paprika, beta carotene, saffron, turmeric, riboflavin, chlorophyll, and caramel (Stevens, Burgess, Stochelski, & Kuczek, 2015).
Overall, focusing on whole and minimally processed foods is beneficial for all your family members and a good way to avoid consuming artificial dyes.
If you would like more information, the Center for Science and Public Interest has an informative website with additional information: Food Dyes: A Rainbow of Risks.
References
Arnold, L. E., Lofthouse, N., & Hurt, E. (2012). Artificial food colors and attention-deficit/hyperactivity symptoms: conclusions to dye for. Neurotherapeutics, 9(3), 599-609.
Arnold, L. E. (2016, February 24). Food dyes and hyperactive behavior in children. Pysch Central. https://pro.psychcentral.com/food-dyes-and-hyperactive-behavior-in-children/
Centers for Disease Control and Prevention (CDC). (2020, April 8). Attention-Deficit / Hyperactivity Disorder (ADHD). https://www.cdc.gov/ncbddd/adhd/index.html
Children and Adults with Attention Deficit/Hyperactivity Disorder (CHADD). (2017, March 3). Do Artificial Food Colors Cause ADHD Symptoms?. https://chadd.org/adhd-weekly/do-artificial-food-colors-cause-adhd-symptoms/
Kanarek, R. B. (2011). Artificial food dyes and attention deficit hyperactivity disorder. Nutrition Reviews, 69(7), 385-391.
Kobylewski, S., & Jacobson, M. F. (2010). Food dyes: a rainbow of risks. Center for Science in the Public Interest (CSPI).
McCann, D., Barrett, A., Cooper, A., Crumpler, D., Dalen, L., Grimshaw, K., ... & Sonuga-Barke, E. (2007). Food additives and hyperactive behavior in 3-year-old and 8/9-year-old children in the community: a randomized, double-blinded, placebo-controlled trial. The Lancet, 370(9598), 1560-1567.
Nigg, J.T., Lewis, K., Edinger, T., Falk, M. (2012) Meta-analysis of attention-deficit/hyperactivity disorder symptoms, restriction diet, and synthetic food color additives. Journal of the American Academy of Child Adolescent Psychiatry, 51(8), 86-97.
Potera, C. (2010). Diet and nutrition: the artificial food dye blues. Environmental Health Perspectives, 118(10), A428.
Stevens, L. J., Kuczek, T., Burgess, J. R., Hurt, E., & Arnold, L. E. (2011). Dietary sensitivities and ADHD symptoms: thirty-five years of research. Clinical Pediatrics, 50(4), 279-293.
Stevens, L. J., Burgess, J. R., Stochelski, M. A., & Kuczek, T. (2015). Amounts of artificial food dyes and added sugars in foods and sweets commonly consumed by children. Clinical Pediatrics, 54(4), 309-321.
Trasande, L., Shaffer, R. M., & Sathyanarayana, S. (2018). Food additives and child health. Pediatrics, 142(2), e20181410.
Weiss, B. (2012). Synthetic food colors and neurobehavioral hazards: the view from environmental health research. Environmental Health Perspectives, 120(1), 1-5.
Xu, G., Strathearn, L., Liu, B., Yang, B., & Bao, W. (2018). Twenty-year trends in diagnosed attention-deficit/hyperactivity disorder among US children and adolescents, 1997-2016. JAMA Network Open, 1(4), e181471-e181471.
Must-Have Foods During Pregnancy
Emily Dammon, Dietetic Intern 2017

Expecting a baby is an exciting time. It's an overwhelming, exhausting, thrilling, draining, yet totally exciting time. Everyone you know will offer advice and suggestions on how to go through your pregnancy and what to expect. This is normal and everyone means well, yet it is easy to get lost in the long list of what to do and not do. I believe there are a few necessities that must be incorporated, specifically in your diet, as related to what that sweet bundle of joy needs to grow, thrive, and ultimately have the best start at life.
Using prenatal vitamins is typically recommended, yet does not replace a healthy diet. It is imperative that your diet include certain vitamins and minerals from whole foods, as this is the body's best bet for absorption. Ultimately, a whole foods diet, with lots of fruits and vegetables that eliminates processed foods and sugars will do a body and baby good.
In order to provide yourself and your baby with proper nutrients, include these foods in your daily diet before, during and even after pregnancy!
Fiber-Rich Foods -- Research has recently revealed that a high-fiber diet may beneficially alter a woman's gut bacteria during pregnancy, producing anti-inflammatory substances that suppress asthma-related genes in her baby.(1) There is also research that suggests a high-fiber diet can help reduce your risk of premature death from any cause, likely because it helps to reduce your risk of a number of chronic diseases. This can help you and your baby! Choosing vegetables, nuts, and seeds is a great way to increase fiber in your diet.
Examples:
| Cauliflower | Beans | Peas |
| Root Vegetables | Onions | Chia seeds |
| Flax seeds | Almonds | Brussel sprouts |
Leafy Greens and Broccoli -- One of the most important nutrients to make sure is abundant in your diet before and during pregnancy is folate. Folate has been proven to be particularly important for the development of the nervous system and for preventing neural tube defects (NTDs) in babies. Broccoli and dark green leafy vegetables like spinach and kale are loaded with important nutrients for pregnant women, including folate, fiber, potassium, calcium, iron, and vitamins C, K, and A. Also, note that folate is found naturally in food while folic acid is the synthetic version of folate. There is a big difference between the two-especially for certain people with genes that make it more difficult to process folic acid. For more information, read the blog post "Folic Acid vs. Folate: Part I-the link can be found in reference 2.
Wild Caught Salmon and Sardines -- Eating fish is the best way to get omega-3 fats EPA and DHA, but being aware of the toxic effects of pollutants found in fish is incredibly important. Among the safest in terms of contamination, and the highest in healthy omega-3 fat, is wild-caught Alaskan or sockeye salmon. Enjoying salmon a few times a week will greatly improve your omega-3 status.(3) Omega-3 fat and its derivative, DHA, is so essential to a child's development that if a mother and infant are deficient in it, the child's nervous system and immune system may never fully develop, and it can cause a lifetime of unexplained emotional, learning, and immune system disorders. Salmon also contains an abundance of other nutrients, from vitamin B12 and selenium to protein, calcium, and choline, making them one of the best dietary sources of animal-based omega-3s. Sardines have the most amount of omega-3 fats. They are delicious on toast. You can also supplement your diet with animal-based omega-3s by taking a krill or fish oil supplement.
Organic free range eggs -- Eggs are really a superfood. They are a great source of protein, fat, and other nutrients, most importantly choline. In women who are pregnant, choline plays a vital role in helping to prevent certain birth defects, such as spina bifida, as well as playing a role in brain development. Consuming higher levels of choline during pregnancy is linked to beneficial epigenetic changes in the fetus, including protection from stress-related and metabolic disorders, that likely last into adulthood.(4)
Avocados -- Avocados provide close to 20 essential health-boosting nutrients, including potassium, vitamin E, vitamin K, B vitamins, and folate. They're also one of few foods that contain significant levels of both vitamins C and E and are an excellent source of healthy monounsaturated fat.(5) Avocados are absolutely a superfood. You can add avocados pretty much to anything!
Berries -- Berries are magical little fruit. They are lower in sugar than many fruits and therefore less likely to destabilize your insulin levels. Berries also contain high amounts of vitamin C, which helps in the absorption of iron, and they also have fiber. Berries have been found to have disease-fighting phytochemical which are found to boost your immunity, prevent cancer, protect your heart, as well as prevent seasonal allergies. (6)
Liver -- I enjoy Pate regularly in my diet. Pate is finally chopped or seasoned pureed animal liver. Currently, the Western diet rarely involves eating the organs of animals, we prefer the muscle. Eating the liver, especially, has been done by many cultures and groups of people for centuries. Choosing grass-fed beef liver or free-range chicken liver is the only way to go. Impressively abundant in organ meats from pastured animals, Vitamin A is a catalyst for multiple biochemical processes. Vitamin A is vital for prevention of birth defects, prevention of infection, hormone production, optimal thyroid function, good digestion, good vision, and healthy bones and blood. Without it, your body cannot utilize protein, minerals and water-soluble vitamins. (7) Organ meats provide plentiful Vitamin E, K, D, complex B vitamins, choline, and trace minerals. This is a must in your diet during pregnancy and even after as well. There are many great recipes available, start experimenting!
Vitamin D -- Vitamin D is not a specific food, but optimizing your vitamin D during pregnancy is one the most important things you can do for yourself and your baby. When a child is born deficient in vitamin D, his or her health can be significantly affected in any number of ways. Research confirms there is a lifelong impact of vitamin D deficiency in pregnancy ranging from childhood allergies to asthma, colds and flu, dental cavities, diabetes, and even strokes and cardiovascular disease in later life of the child. (8) I believe vitamin D is as important to pregnant women as folate is. Once you become pregnant, or if you are hoping to become pregnant, visit your doctor and have your vitamin D levels checked. One study revealed that women with low levels of vitamins D and E in early pregnancy are associated with an increased risk of asthma in her child within the first 10 years of life. (9) There is also mounting evidence that vitamin D deficiency in pregnant women is linked with pre-term births. (10) Talk with your doctor and find out the best ways to maximize your consumption of vitamin D.
All of these foods deserve a place in your diet during pregnancy and really before and after as well. As the emotional, mental, and physical rollercoaster ensue, it is a good idea to try to enjoy these short or long 9 months and do what you can to help bring a healthy beautiful baby into this world. You and your baby deserve the best and deserve to great healthy start to the next chapter in life!
References
1. Thornburn, A. et al (2015). Evidence that asthma is a developmental origin disease influenced by maternal diet and bacterial metabolites. Nature Communications. doi: 10.1038/ncomms83201.
2. Vitiello, P. (n.d.). Research & Education Blog. Retrieved April 30, 2017, from http://blog.designsforhealth.com/blog/bid/115121/Folic-Acid-vs-Folate-Part-I
3. Dungan, J. (2012). The Salmon in Pregnancy Study: study design, subject characteristics, maternal fish and marine n-3 fatty acid intake, and marine n-3 fatty acid status in maternal and umbilical cord blood. Yearbook of Obstetrics, Gynecology and Women's Health,2012, 152-153. doi:10.1016/j.yobg.2012.06.1
4. Jiang, X., Yan, J., West, A. A., Perry, C. A., Malysheva, O. V., Devapatla, S., . . . Caudill, M. A. (2012). Maternal choline intake alters the epigenetic state of fetal cortisol-regulating genes in humans. The FASEB Journal,26(8), 3563-3574. doi:10.1096/fj.12-207894
5. Dreher, M. L., & Davenport, A. J. (2013). Hass Avocado Composition and Potential Health Effects. Critical Reviews in Food Science and Nutrition,53(7), 738-750. doi: 10.1080/10408398.2011.556759.
6. Chen, L., Xin, X., Yuan, Q., Su, D. and Liu, W. (2014), Phytochemical properties and antioxidant capacities of various colored berries. J. Sci. Food Agric., 94: 180-188.
7. Razaitis, L. (2005, July 29). The Liver Files. Retrieved May 01, 2017, from https://www.westonaprice.org/health-topics/food-features/the-liver-files/
8. Rodda, C.P., Benson, J.E., Vincent, A.J., Whitehead, C.L., Polykov, A. and Vollenhoven, B. (2015), Maternal vitamin D supplementation during pregnancy prevents vitamin D deficiency in the newborn: an open-label randomized controlled trial. ClinEndocrinol, 83: 363-368. doi:10.1111/cen.127.
9. Allan, K. M., Prabhu, N., Craig, L. C., Mcneill, G., Kirby, B., Mclay, J., . . . Devereux, G. (2014). Maternal vitamin D and E intakes during pregnancy are associated with asthma in children. European Respiratory Journal, 45(4), 1027-1036. doi:10.1183/09031936.00102214.
10. Miller, D. R., Turner, S. W., Spiteri-Cornish, D., Scaife, A. R., Danielian, P. J., Devereux, G. S., & Walsh, G. M. (2015). Maternal vitamin D and E intakes during early pregnancy are associated with airway epithelial cell responses in neonates. Clinical & Experimental Allergy, 45(5), 920-927. doi:10.1111/cea.12490.
How to Tame Hepatitis C Related Liver Dysfunction with Diet and Herbal Remedies
Sara Ross, Dietetic Intern 2019

Hepatitis C,a silent killer with the not so subtle nickname "The Dragon", is running rampant, with more people being diagnosed every year. It's estimated that approximately 71 million people have the disease throughout the world (World Health Organization, 2017). There are treatments out there, like the ones you see on TV targeting "Baby-Boomers", but they are often prohibitively expensive. The fact of the matter is that for the uninsured or underinsured, many cannot access these drugs, which can cost nearly $1000.00 per pill. Taken daily, and sometimes for up to 12-weeks, that adds up to a grand total of $84,000.00, if not more!
This is one of the reasons why each year, approximately 400,000 people die of the disease unnecessarily (Centers for Disease Control, 2019). What happens is the hepatitis C virus can cause liver inflammation, which may lead to fibrosis, cirrhosis, and potentially liver cancer, which may lead to premature death. It is thought that the virus replicates in the liver, causing inflammation on its own. At the same time, the immune system attacks the virus and the liver cells, leaving a path of destruction in its wake known as fibrosis (Hepatitis C Trust, 2019). This prognosis may seem grim, but wait! Even without treatment, you or someone you love who has been diagnosed with hepatitis C can slow the progression of liver inflammation with food, beverages, and traditional herbal preparations. How can this be? Well, let's take a look at some of these alternative ways to combat hepatitis C and its symptoms.
It's Tea Time!
How about some green tea? Yes, the very same green tea that has been coveted and consumed in Asian countries, including China and Japan, for many millennia. It is not just an energizing beverage with a unique flavor, but also an elixir that can tame the hepatitis C "dragon". Tea enthusiasts in the United States and other westernized countries have touted the beverage for its health-related properties for several decades, as well, but until recently, research was minimal on how green tea could help slow the progression of liver inflammation. One study, however, indicated that green tea can combat hepatitis C due to having a high concentration of a plant-based substance called epicatechin. These substances, or polyphenols, not only have antiviral properties but are also anti-inflammatory (Lin et al., 2013). Talk about packing a one-two punch! Granted, this study was conducted in test-tubes, but it gives hope that future human studies will take place to help green tea take its place as an alternative to slow the hepatitis C virus. In the meantime, brew yourself a vibrant cup of green tea.
Coffee
While we're on the subject of caffeinated beverages, let's talk about coffee. Seriously, who doesn't love a nice cup of coffee (or two) in the morning? It gives that much-needed jolt of energy, plus, for many, its enticing aroma and flavors stimulate the senses like no other beverage can. Coffee may jump-start your morning, but what can this stimulating tonic do for the liver? Well, as it turns out, quite a bit. In one study, men who consume as little as 100 mg of caffeine (that's about one six-ounce cup of coffee) can slow and even reverse liver inflammation and fibrosis. The study did compare other caffeinated beverages, including black tea and caffeinated sodas, but coffee was found to be the most effective in taming the symptoms of hepatitis C (Khalaf et al., 2015). In a later study that focused on liver stiffness, coffee again was found to be a powerful beverage for reversing liver dysfunction, with as little as two cups per day (Hodge et al., 2017). Sounds to me like a win-win situation for those who have been diagnosed with hepatitis and who must have that cup (or two) of coffee in the morning.
Plums
Plums are juicy, sweet, slightly tart, and bursting with summer flavor. Also, they are loaded with nutrients, such as vitamins A, C, and K, antioxidants, and are a great source of fiber. In a recent study that tested different fruits and their impact on hepatitis C, it was found that the plum, or Prunus domestica, can prevent the hepatitis C virus from entering the liver cells. You may be wondering, how the lowly plum, a fruit far less popular than summer's other orchard offerings (hello, peach!) have these anti-viral properties. Well, in essence, on top of the bounty of vitamins and minerals, plums contain a substance called rutin, which has recently been found to have anti-inflammatory and anti-viral properties. What the researchers found was that rutin actually blocks the virus from attaching to liver cells. Without being able to go through the initial stage of attachment, the virus is unable to replicate, giving the liver a much better chance of remaining healthy and fibrosis free (Bose, Kamra, Mullick, Bhattacharya, & Das, 2017). Look out peach. Here comes the mighty plum.
Curcumin
Curcumin has been all the rage in the supplement world, and with good reason. It's relatively new as a supplement in the western world, but in India and other countries where Ayurveda is practiced, it has been a medicinal mainstay for thousands of years. From an Ayurvedic perspective, curcumin, a compound which is derived from the beautifully hued spice, turmeric, is found in foods, beverages, and other compounds that address common inflammatory conditions, including those that affect the liver. Now it can be found in tablet and capsule form, in grocery stores, pharmacies, online, and at discount stores. It is everywhere! But how can it help the liver? In two animal-based studies, it was found that curcumin's anti-inflammatory properties can retard the advancement of fibrosis by stepping in the way of inflammatory substances called cytokines. In both studies, not only were levels of inflammation and fibrosis reduced, but also significant reductions were seen for liver enzymes, which when elevated, are a tell-tale sign of advancing liver disease (Kyung et al., 2018; Shibayama, Reyes-gordillo, Vergara, Moreno, & Muriel, 2008). So have your curries with no worries, as you put liver inflammation to rest with curcumin.
Silymarin (Milk Thistle)
Silymarin, which is derived from what is commonly known as milk thistle, has also been used to combat liver dysfunction for thousands of years. Several decades ago, you would be hard-pressed to find milk thistle in any form, outside of health food and supplement stores, but now you can find the herb in pretty much any larger grocery store, and of course online. It can be found in whole or ground seed form, extracts, sachets, powdered protein blends, capsules, and tablets. You name it; it's out there. According to the history tomes, Pliny the Elder (23-79 A.D.) described a concoction of milk thistle and honey as being powerful enough to eliminate excess bile; a substance naturally produced by the liver (Kazazis, Geladardi, Kyriakos, & Valianou, 2016). In more recent years, animal-based research has found that milk thistle is not only an anti-viral but can also reduce free radicals; a by-product in the body that can damage cells, causing inflammation and sometimes cancer. (Makhlouf, Soelm, & Mohmoud, 2014). Let's just say that amazing things can be done with this thorny little weed with the bright pink flower.
Glycyrrhizin
Glycyrrhizin, a peculiar name for the compound found in licorice, is another botanical that has been used for thousands of years as a natural remedy for liver health. Also, like curcumin and silymarin, glycyrrhizin is highly effective as an antiviral and anti-inflammatory. Using human liver samples, in vitro, of patients who were unresponsive to pharmaceutical treatments, it was found that via a complex mechanism, glycyrrhizin, when administered to the liver cells, prevented attachment and replication of the virus ("Antiviral activity of glycyrrhizin against hepatitis C virus in vitro," 2013). In another study involving hepatitis C patients who were non-responsive to pharmaceutical treatments, it was found that after 52-weeks of being administered glycyrrhizin intravenously, significant reductions in inflammatory markers and fibrosis occurred. After 12 weeks, a decrease in liver enzymes was noted, indicating that glycyrrhizin is effective in treating viral liver diseases (Manns et al., 2012). In a more recent study with hepatitis B patients, again, results showed that glycyrrhizin was effective in reducing liver enzymes and inflammatory markers, clearly indicating that glycyrrhizin should continue to be considered as a tool in the arsenal of therapies used against hepatitis C (Peng, Zhang, & Yuan, 2017).
Talk to Your Doctor about Natural Approaches to Hepatitis-C
So there you go. A brief list of natural foods, beverages, and remedies to turn to for hepatitis C related liver dysfunction. When pharmaceuticals aren't available, try one or a combination of these treatments to slow or reverse liver fibrosis to get back on the path to better health. As always, consult with your health practitioner before adding foods, beverages, or supplements to your healthcare regimen, and eliminate alcohol and other inflammatory foods, such as refined sugars and grains.
References
Antiviral activity of glycyrrhizin against hepatitis C virus in vitro. (2013). PLoS ONE, 8(7). https://doi.org/http://dx.doi.org/10.1371/journal.pone.0068992.
Bose, M., Kamra, M., Mullick, R., Bhattacharya, S., & Das, S. (2017). Identification of a flavonoid isolated from plum (Prunus domestica) as a potent inhibitor of Hepatitis C virus entry. Scientific Reports, 7(May), 1-11. https://doi.org/10.1038/s41598-017-04358-5.
Centers for Disease Control. (2019). Hepatitis C Questions and Answers for Health Professionals. Retrieved from https://www.cdc.gov/hepatitis/hcv/hcvfaq.htm.
Hepatitis C Trust. (2019). How hepatitis C damages the liver. Retrieved from http://www.hepctrust.org.uk/information/impact-hepatitis-c-liver/hepatitis-c-and-liver-damage.
Hodge, A., Lim, S., Goh, E., Wong, O., Marsh, P., Knight, V., … Courten, B. De. (2017). Coffee intake is associated with a lower liver stiffness in patients with non-alcoholic fatty liver disease, hepatitis c , and hepatitis b. Nutrients, 9(56). https://doi.org/10.3390/nu9010056.
Kazazis, C., Geladardi, E., Kyriakos, T., & Valianou, N. G. (2016). Milk thistle: New persepctives. Current Topics in Nutraceutical Research, 14(2), 103-108.
Khalaf, N., White, D., Kanwal, F., Ramsey, D., Mittal, S., Tavakoli-tabasi, S., … El-serag, H. B. (2015). Coffee and caffeine are associated with decreased risk of advanced hepatic fibrosis among patients with hepatitis C. Clinical Gastroenterology and Hepatology, 13(8), 1521-1531.e3. https://doi.org/10.1016/j.cgh.2015.01.030.
Kyung, E. J., Kim, H. B., Hwang, E. S., Lee, S., Choi, B. K., Kim, J. W., … Woo, E. J. (2018). Evaluation of hepatoprotective effect of curcumin on liver cirrhosis using a combination of biochemical analysis and magnetic resonance-based electrical conductivity imaging. Mediators of Inflammation, 2018. https://doi.org/htttps://doi.org/10.1155/2018/5491797.
Lin, Y., Wu, Y., Tseng, C., Lin, C., Chen, W., Hsu, Y., & Lee, J. (2013). Green tea phenolic epicatechins inhibit hepatitis c virus replication via cycloxygenase-2 and attenuate virus-induced inflammation. PLOS One, 8(1), 1-10. https://doi.org/10.1371/journal.pone.0054466.
Makhlouf, A. I. A., Soelm, A. M. A., & Mohmoud, M. A. (2014). Antioxidant and hepatoprotective effects of silymarin phytosomes compared to milk thistle extract in CCl 4 induced hepatotoxicity in rats. Journal of Microencapsulation, 2048(1), 23-30. https://doi.org/10.3109/02652048.2013.805836.
Manns, M. P., Wedemeyer, H., Singer, A., Khomutjanskaja, N., Dienes, H. P., Roskams, T., … Study, S. (2012). Glycyrrhizin in patients who failed previous interferon alpha-based therapies: biochemical and histological effects after 52 weeks. Journal of Viral Hepatitis, 19, 537-546. https://doi.org/10.1111/j.1365-2893.2011.01579.x.
Peng, F., Zhang, T., & Yuan, M. (2017). Influence of compound glycyrrhizin on liver functions: Liver fibrosis indexes and inflammatory factors of patients with chronic hepatitis B. Journal of Hainana Medical University, 23(4), 60-64. Retrieved from http://www.hnykdxxb.com.
Shibayama, M., Reyes-gordillo, K., Vergara, P., Moreno, M. G., & Muriel, P. (2008). Curcumin prevents and reverses cirrhosis induced by bile duct obstruction or CCl 4 in rats: Role of TGF-b modulation and oxidative stress. Fundamental and Clinical Pharmacology, 22, 417-427. https://doi.org/10.1111/j.1472-8206.2008.00611.x.
World Health Organization. (2017). Global hepatitis report, 2017. Retrieved from https://www.who.int/hepatitis/publications/global-hepatitis-report2017/en/.
Beat the College Blues
5 Simple Lifestyle Changes to Help Improve Mood and Diminish Depressive Symptoms
Emma Baker, Dietetic Intern 2022

Transitioning from high school to college can be a stressful time in a person’s life. The amount of responsibility increases, the size of your safety net decreases, and expectations of academic performance rise to new levels. On top of that, you might be far away from home and dealing with homesickness. Suddenly, you notice you are feeling unhappy, struggling to go to class, and struggling to meet academic and extracurricular obligations. If this sounds like something you are experiencing, you aren’t alone. According to the CDC, 4.7% of adults over the age of 18 deal with regular depression symptoms (FastStats - Depression, 2021). However, you don’t have to be stuck feeling like this. Most college campuses provide free counseling to full-time students. Furthermore, there are lifestyle changes you can make in addition to counseling that can further improve your mood and feelings of depression.
Don’t Underestimate Healthy Eating
Proper eating and nutrition can be more powerful than you think! I’m sure you’ve heard that healthy eating has a multitude of physical benefits, but did you know that healthy eating can impact mental health as well? One study spanning a length of 12 years found that a higher habitual intake of fruits and vegetables is associated with lower depressive symptoms. Specifically, a higher intake of red, orange, and yellow vegetables, as well as leafy greens, is significantly associated with lower depressive symptoms, even at only 2 servings per day! Additionally, a greater diversity of vegetable intake (>4 types per day) was associated with 24-42% lower odds of having depressive symptoms (Radavelli-Bagatini et al., 2021). You can see that fruit and vegetable intake has a big impact on mental health!
Another study conducted by Lanuza et al. (2021) found an association between an increased intake of seafood and legumes and a decreased risk of depression. Furthermore, studies investigating intake of omega-3 fatty acids, whole grains, vegetables, fruits, nuts, and polyunsaturated fats have found that increased intake of these things is associated with a decreased prevalence of depression and anxiety, and individuals who consumed the most of these types of foods had 80% lower odds of depression when compared to individuals who consumed the least amount of these foods (Rahmani et al., 2017).
It’s obvious that healthy eating and consumption of fruits, vegetables, whole grains, seafood, nuts, and polyunsaturated fatty acids have beneficial effects on depressive symptoms. If you find yourself regularly consuming foods high in sugar and refined carbohydrates, even adding in a few servings of fruits and vegetables a day, as well as a couple of servings of seafood per week, could help improve your mood and may make going through your day a little bit easier. Try to stick to steamed or baked vegetables and avoid fried varieties of seafood!
Rethink the Soda
When you are feeling depressed, you might find yourself craving sugary beverages, specifically soda. Research has found that intake of sugar-sweetened beverages might not be the best choice for your mental health. A meta-analysis conducted by Hu et al. (2019) looked at observational studies investigating the impact of sugar-sweetened beverages on depressive symptoms. This meta-analysis found that sugar-sweetened beverages are associated with an increased risk of depression in both children and adults, and an intake of 3 cans of soda per day can increase a person’s risk of depression by 25%! This information may make you think twice before grabbing that can of soda.
Another study looked at the association between intake of sugar-sweetened beverages and 100% fruit juice and poor mental health. The study found that poor mental health was prevalent in 17.2% of individuals who consumed >1 sugar-sweetened beverage a day compared to 10.2% of individuals who consumed no sugar-sweetened beverages a day, indicating that consuming >1 sugar-sweetened beverage a day was associated with poorer mental health. However, this study did not find a relationship between intake of 100% fruit juice and poor mental health, indicating that the lack of micronutrients in sugar-sweetened beverages may be the biggest contributor to poor mental health (Freije et al., 2021).
Based on this information, you might want to skip the soda next time you’re thirsty! Other alternatives you might consider include sparkling water or powdered water mix-ins that can add a burst of flavor without the extra sugar. Plain water is also a great choice to quench your thirst.
Give Yoga or Aerobic Exercise a Try
I’m sure that when you’re feeling down, some form of exercise is the last thing on your mind. However, it might be the thing you need to help improve your mood. Specifically, yoga or aerobic exercise may be able to help improve your symptoms. One study found that individuals who were assigned to an 8-week Hatha yoga intervention (classical yoga breathing techniques, mindful body postures, and final deep relaxation pose) experienced statistically and clinically significant decreases in their depression severity. In this study, yoga participants were more likely to achieve remission from their mild-to-moderate depression when compared to controls (Prathikanti et al., 2017). Another study investigated the effects of Bikram yoga (hot yoga) and aerobic exercise on depressive symptoms, perceived stress, and repetitive negative thoughts (rumination). This study found that both Bikram yoga and aerobic exercise significantly decreased depressive symptoms, perceived stress, and rumination. In fact, 61% of participants in the yoga group and 60% of participants in the aerobic exercise group met the clinical criteria for remission of their depression (La Rocque et al., 2021). Talk about a positive impact!
You don’t have to exercise 7 days a week to experience improvement in your mental health. Just incorporating exercise 3 to 4 days a week is a great first step to beginning an exercise routine. Many college recreation centers even offer group classes included in your membership! Group classes would be a great way to get exercise in while also meeting new people and creating connections. Other options include YouTube videos or simply going for a walk outside.
Get a Good Night’s Rest
If you are feeling depressed, you may be staying up late doing things that make you feel happy, such as watching TV, playing video games, or scrolling on social media. I know that whenever I’ve felt down in the past, staying up until the early morning to re-watch episodes of my favorite TV show was the only thing that seemed to make me feel any better. However, lack of sleep can actually end up making your symptoms worse.
A study conducted on adolescents aged 13-19 found that those who slept less than 7 hours a night experienced increased odds of depressive symptoms when compared to adolescents who slept an adequate amount, including sadness, irritability, worthlessness, low motivation, difficulty concentrating, inability to feel pleasure from usual interests, anxiety, and thoughts of self-harm and/or suicide. This study considered an appropriate amount of sleep to be 8-10 hours per night (Yeo et al., 2019).
While your TV show, video game, or social media feed may make you feel better, it is only temporary. The lack of sleep will have lasting effects on your mood, so I recommend getting at least 8 hours of sleep per night. It’s also suggested that you make sure you have good sleep hygiene to improve your quality of sleep. Click here to read about why sleep hygiene is important and how you can work to improve it.
Consider a Magnesium Supplement
Did you know that approximately 50% of Americans consume less than the Estimated Average Requirement for magnesium? This is mainly due to the heavily processed nature of modern foods, a decreased intake of fruits and vegetables, and an increased intake of fast food (Costello et al., 2016).
Magnesium deficiency can cause many issues within the body. It can also contribute to depression. A cross-sectional study among U.S. adults using data from NHANES found that magnesium intake and risk of depression were inversely associated, meaning that the more magnesium an individual consumed, the lower the risk that they would develop and/or struggle with depression. This study also found that in individuals without depression, the daily dietary magnesium intake and energy intake were significantly higher than in individuals with depression, indicating that magnesium deficiency plays some role in the etiology of depression (Sun et al., 2019).
Eby & Eby conducted a study where they provided magnesium supplements to 4 different individuals with depression symptoms: one 59-year-old hypomanic-depressive male, one 23-year-old depressive female with a history of a traumatic brain injury, one 35-year-old pregnant female with a history of severe postpartum depression, and one 40-year-old moderately depressed male with a dependence on food, tobacco, alcohol, and cocaine. The 23-year-old female and the 40-year-old male were completely cured of their depressive symptoms within 1 week. The 35-year-old female delivered her baby without experiencing any postpartum depression. The 59-year-old male was able to cure his depressive symptoms within 5 years with a combination of magnesium supplementation and other supplementation support (inulin and indole-3-carbinol). These 4 case studies support the idea that magnesium is extremely important for maintaining mental health and can be a possible prevention and/or treatment for depression (Eby & Eby, 2006).
Finally, a 12-week study conducted by Tarleton et al. (2017) looked at the effect of magnesium chloride on mild-to-moderate depressive symptoms in adults. Group 1 started treatment at week 1 and stopped after week 6, while Group 2 started the treatment at week 7. This study found that after 6 weeks of treatment, the participant’s depression scores were significantly improved. However, during the 6-week period when treatment was not being administered, the participants saw no significant decrease in depressive symptoms. During treatment, improvement in symptoms happened in as little as 2 weeks, indicating that magnesium is a quick and effective treatment for mild-to-moderate depression.
While the direct role that magnesium plays in depression is not well-known, it is obvious that magnesium deficiency can exacerbate depression symptoms. If you are interested in taking a magnesium supplement, consider chelated magnesium, such as magnesium glycinate.
These small changes are not intended to replace traditional counseling. However, implementing these changes in addition to counseling can change college from a dreaded requirement into a fun experience where you can meet lifelong friends and make lasting memories.
References
Centers for Disease Control and Prevention. (2021, September 13). FastStats - Depression. Centers for Disease Control and Prevention. Retrieved November 24, 2021, from https://www.cdc.gov/nchs/fastats/depression.htm
Costello, R. B., Elin, R. J., Rosanoff, A., Wallace, T. C., Guerrero-Romero, F., Hruby, A., Lutsey, P. L., Nielsen, F. H., Rodriguez-Moran, M., Song, Y., & Van Horn, L. V. (2016). Perspective: The case for an evidence-based reference interval for serum magnesium: The time has come. Advances in Nutrition: An International Review Journal, 7(6), 977–993. https://doi.org/10.3945/an.116.012765
Eby, G. A., & Eby, K. L. (2006). Rapid recovery from major depression using magnesium treatment. Medical Hypotheses, 67(2), 362–370. https://doi.org/10.1016/j.mehy.2006.01.047
Freije, S. L., Senter, C. C., Avery, A. D., Hawes, S. E., & Jones-Smith, J. C. (2021). Association between consumption of sugar-sweetened beverages and 100% fruit juice with poor mental health among US adults in 11 US states and the District of Columbia. Preventing Chronic Disease, 18. https://doi.org/10.5888/pcd18.200574
Hu, D., Cheng, L., & Jiang, W. (2019). Sugar-sweetened beverages consumption and the risk of depression: A meta-analysis of observational studies. Journal of Affective Disorders, 245, 348–355. https://doi.org/10.1016/j.jad.2018.11.015
La Rocque, C. L., Mazurka, R., Stuckless, T. J. R., Pyke, K., & Harkness, K. L. (2021). Randomized controlled trial of bikram yoga and aerobic exercise for depression in women: Efficacy and stress-based mechanisms. Journal of Affective Disorders, 280, 457–466. https://doi.org/10.1016/j.jad.2020.10.067
Lanuza, F., Petermann-Rocha, F., Celis-Morales, C., Concha-Cisternas, Y., Nazar, G., Troncoso-Pantoja, C., Lassere-Laso, N., Martínez-Sanguinetti, M. A., Parra-Soto, S., Zamora-Ros, R., Andrés-Lacueva, C., & Meroño, T. (2021). A healthy eating score is inversely associated with depression in older adults: Results from the Chilean National Health Survey 2016–2017. Public Health Nutrition, 1–12. https://doi.org/10.1017/s1368980021004869
Prathikanti, S., Rivera, R., Cochran, A., Tungol, J. G., Fayazmanesh, N., & Weinmann, E. (2017). Treating major depression with yoga: A prospective, randomized, controlled pilot trial. PLOS ONE, 12(3). https://doi.org/10.1371/journal.pone.0173869
Radavelli-Bagatini, S., Anokye, R., Bondonno, N. P., Sim, M., Bondonno, C. P., Stanley, M. J., Harms, C., Woodman, R., Magliano, D. J., Shaw, J. E., Daly, R. M., Hodgson, J. M., Lewis, J. R., & Blekkenhorst, L. C. (2021). Association of habitual intake of fruits and vegetables with depressive symptoms: The ausdiab study. European Journal of Nutrition, 60(7), 3743–3755. https://doi.org/10.1007/s00394-021-02532-0
Rahmani, J., Milajerdi, A., & Dorosty-Motlagh, A. (2017). Association of the alternative healthy eating index (AHEI-2010) with depression, stress and anxiety among Iranian military personnel. Journal of the Royal Army Medical Corps, 164(2), 87–91. https://doi.org/10.1136/jramc-2017-000791
Sun, C., Wang, R., Li, Z., & Zhang, D. (2019). Dietary magnesium intake and risk of depression. Journal of Affective Disorders, 246, 627–632. https://doi.org/10.1016/j.jad.2018.12.114
Tarleton, E. K., Littenberg, B., MacLean, C. D., Kennedy, A. G., & Daley, C. (2017). Role of magnesium supplementation in the treatment of depression: A randomized clinical trial. PLOS ONE, 12(6). https://doi.org/10.1371/journal.pone.0180067
Yeo, S. C., Jos, A. M., Erwin, C., Lee, S. M., Lee, X. K., Lo, J. C., Chee, M. W. L., & Gooley, J. J. (2019). Associations of sleep duration on school nights with self-rated health, overweight, and depression symptoms in adolescents: Problems and possible solutions. Sleep Medicine, 60, 96–108. https://doi.org/10.1016/j.sleep.2018.10.041
Centers for Disease Control and Prevention. (2021, September 13). FastStats - Depression. Centers for Disease Control and Prevention. Retrieved November 24, 2021, from https://www.cdc.gov/nchs/fastats/depression.htm.
Antidepressants Are Not My Only Option?
Paige Pierce, Dietetic Intern 2022

If you are depressed, view antidepressants as a last resort, and want to pursue an alternative approach to treating your symptoms, you have come to the right place! Typically, when people reach their 40s and 50s, they start to have diagnoses of chronic illnesses such as diabetes, cardiovascular disease, and hypertension. Usual medical treatment is seeing a doctor and getting prescribed medicine to either treat or manage symptoms associated with their diagnosis. Although depression is a mental disease rather than physical, it is usually treated the same way, but an individual will receive therapy or counseling in addition to medicine. Although medicine can effectively treat chronic diseases, it may not be the best option for some individuals. The only person who can know what is best for you is you. Since you are reading this blog, I assume that you have considered that antidepressants are not your best option and would like to learn about other treatments. In this article, I will cover five supplements that have been shown to treat depression and reduce symptom severity.
Rhodiola, an herb that helps with depression
If you are like me and think about herbs, you think of adding them to your food instead of eating them by themselves. Rhodiola can be used for both and is not only an herb but an apoptogenic herb, meaning that it has health benefits as one of its special properties, in addition to adding taste to foods. Rhodiola is a plant that originated in Europe and Asia and has been researched for many diseases, including depression. One of the healing properties of rhodiola is that it increases mental progress under stress and relieves temporary tiredness. In addition to providing positive effects on mood balance, this herb has been associated with increasing the elimination of depressive symptoms (Darbinyan et al., 2007). Doses of rhodiola rosea L. given at 340 mg or 680 mg once a day has shown improved symptoms of depression with insomnia, mood balance, and emotional strength. This same trial showed that people who were not given the rhodiola did not show the same improvements. Another example of how this herb works with depression is that when taken as a substitute for antidepressants, people experience better tolerance and fewer side effects (Mao et al., 2015). It should be acknowledged that the people who took this herb reported less symptom relief than those who took sertraline (an antidepressant drug). Although this was the result, the people who took the herb did experience depressive symptoms relief, just not to the extent of the antidepressant. Although this is true, rhodiola provided extra perks that the drug did not, such as better absorption and significantly fewer side effects than the antidepressant (Mao et al., 2015).
Low magnesium levels are associated with depressive symptoms
As of 2018, it was estimated that about 48% of the US population consumes less than the recommended amount of magnesium (DiNicolantonio et al., 2018). Magnesium deficiency is related to depression and depressed people may have lower levels of this mineral. Magnesium is involved in over 300 biochemical processes in our bodies. It is important that we intake a sufficient amount of magnesium so that our bodies can stay healthy and function properly. When looking at the relationship between magnesium intake from food sources in depressed people, it was found that there was a relationship between people who had very low magnesium intake and how people rated depressive symptoms (Tarleton & Littenberg, 2015). You may be asking yourself, how much magnesium do I need to take to treat my depression? I'm glad you asked! One study showed that people given 125-300 mg of magnesium glycinate or taurinate with each meal and at bedtime were successful in depression treatment (Eby & Eby, 2006). People who took magnesium also reported symptom relief in less than seven days.
Omega-3, a healthy fatty acid provides depressive relief
The odds are that if you have heard of omega-3, it was probably associated with inflammation and its role in limiting disease onset by reducing the amount of inflammation in the body. Omega-3 is an essential fatty acid that helps support the outer structure of cells. Low amounts of omega-3 can cause abnormal issues in these structures that can lead to unusual cell activity and immune function (Su et al., 2003). Omega-3s have been researched in mental and neurological disorders, such as schizophrenia and bipolar disorder. Omega-3 has also been reported to have benefits to the body in the absence of disease. In people with depression, omega-3’s greatly decrease symptoms of depression when compared to usual treatment. When given a supplement containing 9.6 grams of omega-3’s, people experienced much lower scores on depression questionnaires after taking the adding supplements. Each supplement taken contained 440 mg of Eicosapentaenoic acid (EPA) and 200 mg of docosahexaenoic acid (DHA) (Su et al., 2003). Other people who used Omega-3 supplements containing 1,050 mg/d of EPA and 150 mg/d of DHA for depression treatment reported a positive relationship between omega-3 in depressive symptoms and that taking omega-3 was of clear benefit (Lesperance et al., 2010).
Eat your leafy greens, they contain the B-vitamin folate!
I think it is safe to assume that if you had the choice to eat green leafy vegetables or French fries, you would probably choose French fries. Sources of folate in the diet are leafy green vegetables and whole-grain or products that have been fortified with folic acid. Before trying a supplement, as nutrition professionals, we encourage people to get folate from food sources such as broccoli, eggs, and beans. If this is not possible, folate can be taken as a supplement. An example of folate and its relationship to depression can be exhibited in Finnish men who were monitored by their folate consumption from food and their depressive symptoms. This experiment revealed that the men who had the lowest folate intake had a higher risk of becoming depressed. This study also analyzed the associations between B-vitamin (cobalamin, riboflavin, and pyridoxine) intake with depression, and no associations were found (Tolmunen et al., 2003). Another study looked at folate intake in different forms, including total folate, natural folate, and synthetic folic acid, in depressed US adults. The results revealed that individuals who intake total and natural folate had depressive symptoms inversely associated with values. However, this finding was not identified in individuals who took synthetic folic acid and presented with depressive symptoms (Zheng et al., 2020). Folic acid is the synthetic form of folate and is commonly added to processed foods to prevent folate deficiency in the general population. Folate, commonly called methylated folate, is the natural form of folate naturally found in food.
SAM-e, an amino acid that works almost as well as antidepressants
Have you heard of SAM-e? SAM-e stands for S-Adenosyl-L-Methionine. It is produced in the body by the amino acid Methionine. SAM-e used alone or with other antidepressant medications has been shown to improve the livelihoods of depressed individuals (Cuomo, 2020). The effects of SAM-e supplementation were observed in review studies conducted during varying time lengths, generally between 2 and 12 weeks, and given at 200-3200 mg doses. This review found that participants tolerated most SAM-e except in a few cases in terms of safety. Researchers reported that side effects of SAM-e if any were dry mouth, constipation, and increased heart rate. Other symptoms found were relatively mild and were found in people who were taking SAM-e and antidepressant medication (selective serotonin reuptake inhibitor or imipramine). To support the safety of this supplement, another study analyzed the effects of oral SAM-e and found that it works rapidly at the onset of action, has negligible side effects, and can be used as a safe antidepressant treatment (De Vanna & Rigamonti, 1992).
In conclusion, many alternative supplements can be taken to combat depression that reduces symptom severity. Now the question is, which one should you try? The answer is, there is no right answer! Based on the information you learned in the blog, I suggest that you take your pick! If you only want to try one or all of the supplements listed above, that is fine. If you want to try all of them, I recommend that you try one at a time to see which supplements work for you alone before using them in conjunction with the others. Side effects are always a possibility, so make sure you research side effects before purchasing the supplements you want to try. Work with your health care practitioner, and do not stop taking a medication without first consulting your prescribing physician. I hope that one of these supplements works for you and that you are one step away from having brighter days!
References
Arnold, O., Saletu, B., Anderer, P., Assandri, A., Di Padova, C., Corrado, M., & Saletu-Zyhlarz, G. M. (2005). Double-blind, placebo-controlled pharmacodynamic studies with a nutraceutical and a pharmaceutical dose of ademetionine (SAMe) in elderly subjects, utilizing EEG mapping and psychometry. European Neuropsychopharmacology, 15(5), 533-543.
Cuomo, A., Beccarini Crescenzi, B., Bolognesi, S., Goracci, A., Koukouna, D., Rossi, R., & Fagiolini, A. (2020). S-Adenosylmethionine (SAMe) in major depressive disorder (MDD): a clinician-oriented systematic review. Annals of General Psychiatry, 19(1), 1-7.
Darbinyan, V., Aslanyan, G., Amroyan, E., Gabrielyan, E., Malmström, C., & Panossian, A. (2007). Clinical trial of Rhodiola rosea L. extract SHR-5 in the treatment of mild to moderate depression. Nordic Journal of Psychiatry, 61(5), 343-348.
De Vanna, M., & Rigamonti, R. (1992). Oral S-adenosyl-L-methionine in depression. Current therapeutic research, 52(3), 478-485.
DiNicolantonio, J. J., O’Keefe, J. H., & Wilson, W. (2018). Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis. Open Heart, 5(1), e000668.
Eby, G. A., & Eby, K. L. (2006). Rapid recovery from major depression using magnesium treatment. Medical Hypotheses, 67(2), 362-370.
Lespérance, F., Frasure-Smith, N., St-André, E., Turecki, G., Lespérance, P., & Wisniewski, S. R. (2010). The efficacy of omega-3 supplementation for major depression: a randomized controlled trial. The Journal of Clinical Psychiatry, 71(8), 6074.
Mao, J. J., Xie, S. X., Zee, J., Soeller, I., Li, Q. S., Rockwell, K., & Amsterdam, J. D. (2015). Rhodiola rosea versus sertraline for major depressive disorder: A randomized placebo-controlled trial. Phytomedicine, 22(3), 394-399.
Su, K. P., Huang, S. Y., Chiu, C. C., & Shen, W. W. (2003). Omega-3 fatty acids in major depressive disorder: a preliminary double-blind, placebo-controlled trial. European Neuropsychopharmacology, 13(4), 267-271.
Tarleton, E. K., & Littenberg, B. (2015). Magnesium intake and depression in adults. The Journal of the American Board of Family Medicine, 28(2), 249-256.
Tolmunen, T., Voutilainen, S., Hintikka, J., Rissanen, T., Tanskanen, A., Viinamäki, H., ... & Salonen, J. T. (2003). Dietary folate and depressive symptoms are associated in middle-aged Finnish men. The Journal of Nutrition, 133(10), 3233-3236.
Zheng, L., Yu, X., Jiang, W., & Zhang, D. (2020). Total folate, natural folate and synthetic folic acid intake associations with adult depressive symptoms. Asia Pacific Journal of Clinical Nutrition, 29(4), 846-855.
5 Supplements to Improve Anxiety
Melinda Cloudy, Dietetic Intern 2020

Anxiety disorders affect a whopping 40 million adults in the US making it one of the most common mental illnesses. That is 18.1% of the country's adult population! To make matters worse, about 63% of those suffering do not receive treatment (Anxiety and Depression Association of America, 2018). There are numerous treatments out there that can make a significant impact on the quality of life of someone with an anxiety disorder. Safe treatment for anxiety disorders may be achievable by taking the right supplements. In this post, we'll discuss some of these options, what the research says, and how they can help you.
How Can a Supplement Help with Anxiety?
Anxiety can be caused by a lot of different reasons. Anxiety can be related to how your body functions, your diet, your environment, or your lifestyle. With many causes for anxiety, there seems to be just as many if not more treatments - anything from medication to acupuncture. But I'm not writing this blog to tell you about the wonders of getting poked by needles - I'm writing this to tell you about the wonders of nutrition. There is a huge connection between nutrients and mental health. Moreover, there is a lot of scientific evidence showing how powerful a role nutrition can play in neurological issues such as anxiety. However, it is not always as simple as eating more of a certain food or finding the right diet. Sometimes the only way for a certain nutrient to be therapeutically effective is by taking a supplement.
The Excitatory Area of Neurotransmitters
Before we get going with the supplements, I want to provide a little background into how these supplements work. One of the ways many of the following supplements work is by affecting neurotransmitters in the body. Neurotransmitters are chemicals that send messages to and from the nervous system. Neurotransmitters do tons of vital things including helping us think, moving muscles, feeling pain, and breathing. Additionally, they play a major role in neurological health such as anxiety and depression.
The two main jobs of neurotransmitters are excitation and inhibition. Excitatory neurotransmitters tell your body to do something. Inhibitory neurotransmitters tell your body not to do something (another way of thinking about it is they tell your body to relax) (Berry & Hammond, 2019).
GABA
When it comes to anxiety, the neurotransmitter known as GABA (gamma-aminobutyric acid if you want to be fancy) is extremely important. You can think of GABA as a brake, where one of its jobs is to keep your brain from getting too excited. Of course, there is nothing wrong with your brain getting excited, that is an important part of how the body can function. But when the balance of neurotransmitters that excite to neurotransmitters that relax is thrown off, then mood disorders can result. In fact, scientists have linked low GABA in the brain to anxiety, restlessness, depression, and insomnia (Weeks, 2009).
Additionally, many common medications to treat anxiety such as benzodiazepines and barbiturates function by controlling GABA release and GABA receptors. Some of the supplements I will discuss work because they help GABA do its job. They function similarly to these medications because of their impact on GABA, however, without some of the unseemly side effects of anti-anxiety medication, such as addiction. Now that we've got some of the background out of the way, let's dive into the supplements.
1. Gold Star: Niacinamide
That's right! And it's called niacin. We're going to specifically look at the form called niacinamide for supplement purposes. Niacinamide plays a really important role in serotonin production (serotonin is a neurotransmitter that helps regulate mood) and it acts similarly to medications called benzodiazepines (commonly used to treat issues like anxiety).
Now, a full-blown vitamin B3 deficiency leads to a serious illness called pellagra, but this is pretty rare in America and other developed countries. However, researchers think that many people may be suffering from a slight B3 deficiency that is not serious enough to cause pellagra but is still causing symptoms such as anxiety, depression, fatigue, and GI issues. They also speculate that due to internal and genetic factors, some people may need more niacin than they can get from food alone, making supplementation necessary (Prousky, 2005).
Not to be confused with niacin supplements, niacinamide has been successful in many experiments for treating anxiety. In one case study, an 11-year-old girl, a 28-year-old woman, and a 42-year-old woman with anxiety disorders were prescribed doses of niacinamide ranging from 2000 mg to 2,500 mg per day. All three patients noted significant improvements in their anxiety symptoms with the treatment (Prousky, 2005). Furthermore, in his textbook Nutritional Medicine, Dr. Alan Gaby reports good results with niacinamide supplementation of 500 mg twice a day up to 1000 mg three times a day in his patients with anxiety (Gaby, 2017).
A few important side effects to note: niacinamide may cause upset stomach, gas, dizziness, itching, or rashes. Also, in rare cases, it causes liver problems. Therefore, it is recommended to get regular liver function tests for anyone taking more than 1500 mg per day (Gaby, 2017; NIH, 2019).
2. L-Theanine - Found in Tea and…Fungus?
L-theanine is a pretty amazing amino acid that you get by sipping tea or munching on the Bay Bolete mushroom. It's been in the spotlight recently because of its relationship with neurotransmitters. It seems to reduce anxiety by affecting the release of two important neurotransmitters: dopamine (signals pleasure) and serotonin (inhibits/relaxes) (Yoto et al., 2012).
A study from 2007 using a small sample of male participants tested L-theanine's ability to decrease stress by measuring stress levels during and after the participants engaged in a stress-inducing mental math game. When participants were given 200 mg of L-theanine before the math game, they had reduced levels of stress during the game compared to when they did not take L-theanine (Kimura et al., 2007).
Although it is present in tea, the amount of L-theanine used in studies (around 200 mg) is higher than the amount in 4 cups of tea (and the amount of L-theanine per cup is variable). Drinking too much tea can have other side effects, for one because of the caffeine, therefore, it is probably best to use a supplement.
3. Magnesium
Magnesium is already known to be lacking in many Americans' diets. It is estimated that 68% of Americans are not consuming the recommended amount, which has lots of negative effects. Magnesium plays an important role in mood disorders, and not having enough contributes to anxiety and poor stress tolerance (Boyle, Lawton, & Dye 2017; Gaby, 2017). Additionally, stress and anxiety can increase the body's need for magnesium. It's a cycle, where low magnesium makes you stressed, and being stressed makes you use up more magnesium which just makes you more stressed (Gaby, 2017).
Researchers think magnesium is effective for reducing anxiety because it increases GABA activity helping prevent excess excitation (or agitation) of the brain (Boyle, Lawton, & Dye 2017).
Clearly, it is important that we get enough magnesium, and a supplement is an effective way to do so. Magnesium supplements commonly come as either magnesium citrate or magnesium glycinate. Either would be appropriate, although magnesium citrate may cause diarrhea.
One fun way you can experience the relaxing effects of magnesium is to soak in a warm bath with 1 cup of Epsom salt added to the water. The magnesium in Epsom salt will absorb into your skin helping you relax and even helping you sleep if you do it before bed (Scott, 2011).
Magnesium and Its Buddy B6
Vitamin B6 (aka pyridoxine) has also been shown to help with anxiety and pairing it with magnesium may be better than taking either one alone. Researchers experimented with comparing a supplement of 470 mg of magnesium vs a supplement of 5 mg vitamin B6 plus 470 mg of magnesium. They found that for the subjects who started the trial with the highest level of anxiety, the most significant improvement occurred with the magnesium and B6 supplement. However, when looking at all of the participants together, there was an almost 48% reduction in stress, showing that either treatment may be beneficial (Pouteau et al., 2018). Clearly, taking a supplement of magnesium or magnesium and pyridoxine may be one natural way to help your mental health.
4. How About a B Vitamin Casserole Instead?
As we've seen above, B vitamins play an important role in mental health, but it doesn't stop with B3 and B6. Vitamins B9 (folate) and B12 (cobalamin) are also associated with psychiatric disorders (Turksoy et al., 2014). Rather than supplementing the vitamins individually, it may be more effective to use a high-quality vitamin B complex supplement (Gaby, 2017).
In a study from 2013, participants were supplemented with Max Stress B (containing 1 mg Thiamin, 1.6 mg riboflavin, 30 mg niacinamide, 3 mg pyridoxine, 1000 mcg folate, 263 mg B12, 334 mcg biotin, 3.3 mg pantothenic acid, PABA, inositol) or a placebo for 60 days. Participants had marked improvement in anxiety scale score and mental health score after taking the supplement and did not report any side effects (Lewis et al., 2013).
The Supplement Matters
A lot of the B-vitamins work together, so taking a B complex is a great choice to help you get the appropriate amounts of B vitamins in relation to each other, but even so, picking the right supplement can make a difference in how well this treatment works (Scott, 2011).
Lots of times, vitamins with B9 contain a form called folic acid. This is fine, but a good chunk of the population is unable to use this form of B9 due to genetics (Dean, 2012). Unless you have done genetic testing and are certain that you can utilize folic acid, it is better to purchase a supplement that contains the active form, methylfolate (which works for anyone). Similarly, look for the form of B12 methylcobalamin because that one is easier for the human body to use. While you're at it, pair magnesium with your B vitamin casserole too, and cover all your bases.
5. Ashwagandha, Important Enough to Learn to Pronounce
If you think ashwagandha is a hard word to say, then you can always call the herb by its literal name - "smell of horse." The choice is yours. Jokes aside, this smelly supplement has some real potential (don't be intimidated by that name, just get it as a capsule and leave the horse to be smelt by others) (Chandrasekhar et al., 2012).
Ashwagandha is a special kind of herb known as an adaptogen. Basically, adaptogens make the body better at handling stress. These herbs help decrease bodily damage from stress without withdrawal symptoms or troublesome side effects. Ashwagandha is not the only beneficial adaptogen out there, but it is well known, accessible, and backed by science. Researchers think ashwagandha may be able to mimic the neurotransmitter GABA. (Chandrasekhar et al., 2012).
Ashwagandha has gained popularity in America recently, but it has been effectively used as part of traditional Indian medicine for centuries (Andrade et al., 2000). Several studies have specifically looked at how well ashwagandha helps with anxiety disorders. Using doses of 1 to 2.5 grams per day, there was significant effectiveness in improving anxiety, and no adverse effects were noted by participants (Andrade, 2009).
Another study took 39 participants with diagnosed anxiety disorders and gave half of them ashwagandha extract and half a placebo for 6 weeks. The doses were adjusted based on how participants responded to treatment and ranged from 0.5 to 2.5 grams of ashwagandha. By the end of the trial, the ashwagandha group's anxiety levels were significantly improved compared to the placebo (Andrade, 2009).
And if you weren't convinced and needed just one more positive study to get you there, then 64 subjects with a history of chronic stress were given 300 mg Ashwagandha or a placebo for 60 days. Those taking ashwagandha experienced significant improvements on the depression anxiety stress scale, with an improvement from a score of 16 to 4 for anxiety specifically (Chandrasekhar et al., 2012).
Conclusion
As you were hopefully able to see from this post, there are so many natural supplements to help with anxiety, that no one should have to suffer through it without help. If you are concerned about side effects of medication or have been unsuccessful with previous treatment, then there are still options for you to try. This post highlighted some nutritionally-sound, science-backed, safe treatments for anxiety. Remember, this post is not meant to replace professional medical advice. It is important to discuss any alternative treatments you are interested in with a qualified health professional so they can help monitor and guide you. Please click here to sign up for regular emails about what you eat and your mental health.
References
Andrade, C. (2009). Ashwagandha for anxiety disorders. The World Journal of Biological Psychiatry, 10(4-2), 686-687.
Andrade, C., Aswath, A., Chaturvedi, S. K., Srinivasa, M., & Raguram, R. (2000). A double-blind, placebo-controlled evaluation of the anxiolytic efficacy of an ethanolic extract of withania somnifera. Indian Journal of Psychiatry, 42(3), 295.
Anxiety and Depression Association of America. (2018). Facts and Statistics. https://adaa.org/about-adaa/press-room/facts-statistics
Berry, J. & Hammond, N. (2019, October 11). What are neurotransmitters. Medical News Today. https://www.medicalnewstoday.com/articles/326649
Boyle, N. B., Lawton, C., & Dye, L. (2017). The effects of magnesium supplementation on subjective anxiety and stress-a systematic review. Nutrients, 9(5), 429.
Chandrasekhar, K., Kapoor, J., & Anishetty, S. (2012). A prospective, randomized double-blind, placebo-controlled study of safety and efficacy of a high-concentration full-spectrum extract of ashwagandha root in reducing stress and anxiety in adults. Indian Journal of Psychological Medicine, 34(3), 255.
Dean, L. (2012). Methylenetetrahydrofolate reductase deficiency. Medical Genetics Summaries, 409.
Gaby, A. R. (2017). Nutritional Medicine. (2nd ed.). Fritz Perlberg Publishing. https://adaa.org/about-adaa/press-room/facts-statistics
Kimura, K., Ozeki, M., Juneja, L. R., & Ohira, H. (2007). L-Theanine reduces psychological and physiological stress responses. Biological psychology, 74(1), 39-45.
Lewis, J. E., Tiozzo, E., Melillo, A. B., Leonard, S., Chen, L., Mendez, A., ... & Konefal, J. (2013). The effect of methylated vitamin B complex on depressive and anxiety symptoms and quality of life in adults with depression. ISRN Psychiatry, 2013.
National Institutes of Health. (2019, April 9). Niacinamide. MedlinePlus. https://medlineplus.gov/druginfo/natural/1534.html#top
Pouteau, E., Kabir-Ahmadi, M., Noah, L., Mazur, A., Dye, L., Hellhammer, J., Pickering, G., & Dubray, C. (2018). Superiority of magnesium and vitamin B6 over magnesium alone on severe stress in healthy adults with low magnesemia: A randomized, single-blind clinical trial. PloS One, 13(12), e0208454. https://doi.org/10.1371/journal.pone.0208454
Prousky, J. E. (2005). Supplemental niacinamide mitigates anxiety symptoms: three case reports. Journal of Orthomolecular Medicine, 20(3), 167-178.
Scott, T. (2011). The anti-anxiety food solution: How the foods you eat can help calm your mind, improve your mood, and end cravings. New Harbringer Publications, Inc.
Turksoy, N., Bilici, R., Yalçiner, A., Ozdemir, Y. Ö., Ornek, I., Tufan, A. E., & Kara, A. (2014). Vitamin B12, folate, and homocysteine levels in patients with obsessive-compulsive disorder. Neuropsychiatric Disease and Treatment, 10, 1671-1675. https://doi.org/10.2147/NDT.S67668
Weeks, B. S. (2009). Formulations of dietary supplements and herbal extracts for relaxation and anxiolytic action: Relarian. Medical Science Monitor, 15(11), RA256-RA262.
Yoto, A., Motoki, M., Murao, S., & Yokogoshi, H. (2012). Effects of L-theanine or caffeine intake on changes in blood pressure under physical and psychological stresses. Journal of Physiological Anthropology, 31(1), 28.
Alzheimer's Disease and Insulin Resistance: What Is the Link? A Poor Memory Is More Serious Than You Think
SooYoung Lackey, Dietetic Intern 2020

Lidia (24) is a graduate school student who is managing two jobs and school at the same time. Graduate school is not easy; however, she is proud of how far she has come and is excited about what awaits her in the future. It was only about two months ago that Lidia started to feel like she was getting behind on things. She started to forget what time she was supposed to be at work, her phone number, and her homework due dates. When she had a day off from work and school, she would sleep throughout the day without any intention of doing so. Her productivity slowly dwindled, and she began having trouble just catching up with her daily tasks. When she visited a doctor, her doctor told her that she was prediabetic and that now she needed to control her diet. Her doctor mentioned that she did not need to worry too much about her brain function because she is still young and that she might be just a little too stressed out. Just like that, without really knowing how to help her brain, Lidia tried to continue her daily life.
Lidia is only 24 years old, she has been actively using her brain by furthering her knowledge, so why is she already experiencing cognitive decline? Why does she forget little yet important things and sleep through her days off? Is it possible that she might be developing some sort of neurological disease at an early age? But aren't neurological diseases, like Alzheimer's disease, only prevalent in the elderly?
Interestingly, research suggests that age-related cognitive decline begins in healthy and educated adults when they are in their 20s or 30s, and can go unnoticed until they are actually diagnosed with disease (Salthouse, 2009). Can you believe it? According to a survey done by the American Association of Retired Persons (AARP) in 2015, 1,200 Americans were interviewed regarding the importance of brain health and 98% of the interviewees answered that they thought brain health matters extremely. The problem was that less than 50% knew how to help their brain. Some of us might be thinking medication is the only real way to help Alzheimer's disease, but that might not be the case. A study from Cummings et al., (2014) reported that Alzheimer's drug trials have a 99.6% failure rate. Ninety-nine percent failure rate? Looking at that, you could easily say that treating Alzheimer's disease with conventional medication might not be the best way to slow the progress of the disease. So, if we cannot treat it with medication, is there a way we can prevent Alzheimer's disease?
Insulin Resistance and Alzheimer's Disease
Researchers claim that one in three Alzheimer cases are preventable by reducing the risk factors, such as diabetes (Norton et al., 2014). According to the Mayo Clinic, diabetes and Alzheimer's disease are linked, indicating that poor insulin sensitivity increases the risk for Alzheimer's disease (Mayo Clinic, 2017). For most, it may not be surprising to hear of a patient with poorly controlled type 2 diabetes, having some form of cognitive impairment, such as mental flexibility, memory, and mental speed. Cognitive impairment found in type 2 diabetes can progress to Alzheimer's disease by inducing vascular dysfunction and oxidative stress. A study done on elderly people in China reported that out of 197 participants with type 2 diabetes, 115 of them had either mild cognitive impairment or Alzheimer's disease (Li et al., 2016). Gathering from that study, we can see that there is some sort of connection between these two different diseases. What is the link between Alzheimer's disease and diabetes? How come some people are calling Alzheimer's disease "type 3 diabetes"? Maybe, it has to do with insulin function!
We know that diabetes occurs when your body cannot make or effectively use insulin. Insulin signaling pathways work in various types of cells and tissues to regulate energy metabolism, homeostasis, and the reproduction system. It was found that beyond all these listed roles, insulin also modifies neuronal activity, and improves memory function in the brain. Insulin seriously does way more than we think! Data from many different studies have reinforced that the brain is an insulin-sensitive organ (Fernandez & Torres-alemán, 2012). So, just what could happen if you have insulin resistance?
5 Ways How Insulin Resistance Can Cause Alzheimer's Disease
Before discussing more deeply about insulin resistance and Alzheimer's disease, I want to explain the pathophysiology of Alzheimer's disease. According to Imbimbo et al., (2013) Alzheimer's disease can be characterized by the build-up of amyloid-ß (Aß) plaque and neurofibrillary tangles (NFT) in the nerve cells. In healthy neurons, there is a natural protein called the Tau protein, which maintains the integrity of cellular microtubules. However, the Tau protein is hyperphosphorylated in patients with Alzheimer's disease due to oxidative stress, causing deterioration of microtubules in the nerve cells. The hyperphosphorylated tau protein forms NFT, which gets distributed throughout the body of the nerve cell and causes problems. Amyloid plaque builds up between nerve cells due to mutase in gamma-secretase and mutated gamma-secretase lets amino acid peptide fragments of amyloid precursor protein (APP) longer than 42 into the nerve cell, causing Aß plaque. Now that we've gone over that, let's talk more about the relationship between insulin resistance and Alzheimer's disease (Imbimbo, Lombard, & Pomara, 2005).
Mittal et al., (2016) described 5 possible routes of how insulin resistance can progress Alzheimer's disease.
1. Both diabetes and Alzheimer's disease have up-regulation of an Insulin degrading enzyme (IDE)
Increased levels of IDE down-regulate insulin growth factor -1 (IGF-1), which further increases the activity of interleukin-1 beta (IL1B). Too much IL1B produces oxidative stress in the brain. Oxidative stress is one main cause of the formation of NFT in the nerve cells. IL1B affects the activity of apolipoprotein E (APOE), which is involved in the formation of amyloid precursor protein (APP). It is known that amyloid- ß plaque is one of the characteristics of patients with Alzheimer's disease.
2. Insulin resistance causes disturbance in the insulin signaling pathway
Disturbance in the insulin signaling pathway eventually causes dephosphorylation of the Bc12-associated agonist of cell death (BAD) protein, which triggers the apoptosis process. By initiating cell death in patients with Alzheimer's disease, the BAD protein causes mitochondrial dysfunction, resulting in amyloid- ß plaque formation.
3. Decreased insulin signal causes decreased expression of low-density lipoprotein 2 (LRP2)
Low-density lipoprotein 2 (LRP2) plays a role in the retention of insulin from the kidney. However, when the insulin signal has been decreased, LRP2 is also decreased in its expression, eventually causing up-expression of apolipoprotein (APOE), resulting in the formation of amyloid- ß plaque.
4. Insulin resistance inhibits retinoblastoma protein (RB)
RB protein facilitates adipocyte differentiation by forming a complex with insulin. However, insulin resistance leads to disturbance in forming this complex, and eventually affects the RB protein in a way that alpha-synuclein (SNCA) protein, which is primarily found in neural tissue, interacts with the formation of amyloid- ß plaque in the brain.
5. Impairment in the insulin signaling reduces the affinity of insulin for the insulin receptor
When insulin signaling is impaired, there is an alteration in the interaction between insulin receptors with insulin receptor substrate 1(IRS1) and insulin receptor substrate 2 (IRS2). This altered interaction affects fat metabolism, and eventually causes amyloid- ß production (Mittal, Mani, & Katare, 2016).
These five different reasons only explain a few possible ways of how insulin resistance can cause Alzheimer's disease. As you can see, insulin resistance and amyloid-ß plaque have deep relationships. Considering the formation of amyloid- ß plaque and neurofibrillary tangles (NFT) in the nerve cells are two of the main characteristics of Alzheimer's disease, insulin resistance is something to be more aware of. Lidia may have thought she was just like everyone else until she was diagnosed as prediabetic. How many people are unaware of the fact that they might have diabetes or insulin resistance? As Salthouse, (2009) mentioned in their study, cognitive decline starts in healthy individuals from their 20s. This should alarm us! Alzheimer's disease does not only apply to the elderly generation anymore. We are living in a world full of refined carbohydrates. During this day and age, many of us do not need to labor too much to get our work done, nor hunt for food. Most of the time, we are sitting down, working on the computer or phone. We can just get in a car, go to a fast-food restaurant, and grab what we want to eat through a drive-thru window. People are more unhealthy than ever before, and more people are diagnosed with diabetes than ever before, which means you might potentially be developing insulin resistance without showing any symptoms at this moment.
Okay I'm Listening. What Should I Do?
The first step towards a healthy brain is to be considerate of your brain and learn how to help it. One thing to remember is that everyone is different, and therefore, there is no 'one diet' or 'one supplement' to help your brain. I propose we try taking one small step at a time. In this blog, we have discussed how insulin resistance can be a trigger for developing Alzheimer's disease. There are several ways to help increase insulin sensitivity that you might benefit from. Here is a list of a few very simple changes that you can apply to your life.
Think about how much and what you are eating throughout the day.
- Reducing the total carbohydrates from your diet and increasing the total fruit and vegetable intake can increase insulin sensivity (Krebs et al., 2013).
- Try not to get too full when you eat. Consider portion sizes!
- Intermittent fasting can help control your blood sugar (Tello, 2020).
Increase your daily physical activity.
- Increased levels of habitual physical activity in moderate amounts have shown positive effects on insulin resistance (Venkatasamy, Pericherla, Manthuruthil, Mishra, & Hanno, 2013).
- If you aren't ready for moderate physical activity, start with a walk in the park, consider taking the stairs instead of an elevator. Small things like these can change your habits!
These are just simple suggestions that you can choose to follow, however, if you feel like your brain function isn't where it needs to be, then do not hesitate to contact your doctor or local dietitian for help!
References
Brain health important to 93% of Americans, but few know the 5 ways to help maintain or improve it (2015, January 20). AARP. Retrieved April 18, 2020, from https://press.aarp.org/2015-01-20-Brain-Health-Important-to-93-of-Americans-But-Few-Know-the-5-Ways-to-Help-Maintain-or-Improve-It#assets_all
Cummings, J. L., Morstorf, T., & Zhong, K. (2014). Alzheimer's disease drug-development pipeline: Few candidates, frequent failures. Alzheimer's Research and Therapy, 6(4), 1-7. https://doi.org/10.1186/alzrt269
Fernandez, A. M., & Torres-alemán, I. (2012). The many faces of insulin-like peptide signalling in the brain. 13(April), 225-239. https://doi.org/10.1038/nrn3209
Imbimbo, B. P., Lombard, J., & Pomara, N. (2005). Pathophysiology of alzheimer's disease. Neuroimaging Clinics of North America, 15(4), 727-753. https://doi.org/10.1016/j.nic.2005.09.009
Krebs, J. D., Bell, D., Hall, R., Parry-Strong, A., Docherty, P. D., Clarke, K., & Chase, J. G. (2013). Improvements in glucose metabolism and insulin sensitivity with a low-carbohydrate diet in obese patients with type 2 diabetes. Journal of the American College of Nutrition, 32(1), 11-17. https://doi.org/10.1080/07315724.2013.767630
Li, W., Wang, T., & Xiao, S. (2016). Type 2 diabetes mellitus might be a risk factor for mild cognitive impairment progressing to Alzheimer's disease. Neuropsychiatric Disease and Treatment, 12, 2489-2495. https://doi.org/10.2147/NDT.S111298
Mittal, K., Mani, R. J., & Katare, D. P. (2016). Type 3 diabetes?: cross talk between differentially regulated proteins of type 2 diabetes mellitus and alzheimer ' s disease. Nature Publishing Group, 1-8. https://doi.org/10.1038/srep25589
Norton, S., Matthews, F. E., Barnes, D. E., Yaffe, K., & Brayne, C. (2014). Potential for primary prevention of Alzheimer's disease: an analysis of population-based data. The Lancet Neurology, 13(8), 788-794. https://doi.org/10.1016/S1474-4422(14)70136-X
Salthouse, T. A. (2009). When does age-related cognitive decline begin? Neurobiology of Aging, 30(4), 507-514. https://doi.org/10.1016/j.neurobiolaging.2008.09.023
Venkatasamy, V. V., Pericherla, S., Manthuruthil, S., Mishra, S., & Hanno, R. (2013). Effect of physical activity on insulin resistance, inflammation and oxidative stress in diabetes mellitus. Journal of Clinical and Diagnostic Research?: JCDR, 7(8), 1764-1766. https://doi.org/10.7860/JCDR/2013/6518.3306
Can Nutrition and Lifestyle Help Your Anxiety Disorder?
Cristal Hernandez, Dietetic Intern 2020

Have you ever wondered why your anxiety disorder seems untreatable? Constantly hoping that one day all the feelings of misery and worry will go away. You just want to be normal and enjoy life, but it is a constant battle with your head every single day. You even start to feel worse and guilty because you begin to think the way you are affects those around you. This then leads to isolation because you don't want to be a bother to your friends and family. After all the medications and therapy and tests and you still can't find an answer for your anxiety? In my functional nutrition program, we talk about finding the underlying cause and treating it with nutrition. What is causing all the anxiety and where did it come from? The purpose of the following blog will touch on my findings on how to manage anxiety with lifestyle and nutrition.
Where My Interest Stems From
I remember my first few dates with my husband, he would get this weird cough every time we went out to social events. He would get a scratchy throat and would just kind of shake his head in hopes that it had passed. NOPE. Wrong. This "episode" we'll call it went on for as long as it could until he won the battle and finally got past it. I would try to comfort him and try to hold his hand where he would just quickly snatch his hand away with irritability and anger. He would keep his head down, muscles tense, and would then go on to tell me to stop because I wasn't helping. This was hurtful at first. I had never met someone with an anxiety disorder, so I have never really known what to do.
Statistics
According to the Anxiety and Depression Association of America (ADAA), anxiety disorders are the most common mental illness in the U.S., affecting 40 million adults in the United States age 18 and older, or 18.1% of the population every year. Everyone experiences a certain amount of anxiety and fear when faced with a stressful situation. However, when anxiety becomes excessive or prolonged it can become a chronic health condition. It is no longer the simple and usual worry most people get when they stand in front of people.
But don't worry (pun intended), I am here to provide you with some tips that you could give a try! I'll leave it at this, lifestyle changes do wonders for your mind, body, and overall health.
The Power of Nutrition and Stress on the Gut Microbiota and Anxiety
First off, what is the gut microbiota and how is this relevant to your anxiety? There is a large number of evidence on the impact of nutrition and the health of the gut microbiota. The gut microbiota is this ecosystem in our gastrointestinal tract consisting of a trillion friendly bacteria that are important to our health. When it is imbalanced with bad microorganisms, it can lead to multiple disease states including anxiety.
Studies have shown that when you provide your gut, also known as "the second brain" with the nutrients it needs it alters your brain and behavior. This is because our central nervous system (CNS) (which is our brain and spinal cord) is bidirectionally linked to our enteric nervous system (ENS) (or our gut microbiota). These systems work together in influencing our body, mind, mood, emotions, gut function, and behavior. Thus, "the emerging concept of a microbiota-gut-brain axis suggests that modulation of the gut microbiota may be a tractable strategy for developing novel therapeutics for complex CNS disorders" (Cryan and Dinana, 2012). How do we do that?
1. Avoid Excess Sugar
As healthy gut function has been linked to normal CNS function it can be said that the microbiota is very well involved in anxiety and blood sugar balance. Excessive and "regular intake of a high calorie/sugar-rich diet influences gut microbiota composition" (Jena et al., 2016).
This alteration in the gut microbiota composition will then lead to dysbiosis (gut imbalance) and inflammation which then compromises the gut and brain connection. This then "increases intestinal permeability" (leaky gut) and in turn mental imbalances. In fact, one of the functions of the gut is to synthesize "more than 90% of the body's serotonin" - the hormone responsible for your mood and emotions (Do et al., 2018; Yano et al., 2015).
This is where things become problematic.
Once these systems have been compromised, this is where the root cause of many mental disorders like anxiety may come from. In fact, "dysbiosis and inflammation of the gut have been linked to causing several mental illnesses including anxiety and depression" (Clapp et al., 2017).
As you can see, excess sugar can be problematic on your gut putting your body in a constant stressed and inflammatory state leading to gut imbalances, leaky gut, and increasing your anxiety. In general, inflammation is "reliably elevated in a significant proportion of patients with major depressive disorder (MDD), bipolar disorder, anxiety disorders and post-traumatic stress disorder (PTSD)" (Felger, 2018). If there is any way to avoid getting to the inflammation stage, reducing high sugar intake may be helpful. This will save you from mental imbalances in the long run.
2. Increase Whole Foods
This is not to say you can't have sweets or sugar at all. Enjoy them but prioritize more on nutritious foods. Try replacing highly processed foods with various whole foods rich in vitamins, minerals, and antioxidants that offer many benefits. One of the many benefits that antioxidants can provide is the protective effects they offer your mind and body. Most importantly, your gut microbiota. "Dietary antioxidants confer significant protection to gut epithelial cells from pro-apoptotic oxidant stress" (Miller et al., 2001).
Antioxidants are like the warriors of your body protecting you and your many cells from any harm and damage. This means your brain, nerve, and gut cells are protected avoiding any possible dysbiosis and harm "through the stimulation of the growth of beneficial bacteria and the inhibition of pathogenic bacteria" (Dueñas et al., 2015). This will in turn promote a healthy gut-brain axis connection.
As you can guess by this point, having a low antioxidant dietary intake can become problematic in the long run. Antioxidant intake may be a great form of treatment for anxiety as anxiety is thought to be "correlated with a lowered total antioxidant state" (Xu et al., 2014). What's great is that you can get antioxidants from food!
Antioxidants can be found in spices, beans, apples, nuts, and asparagus. "Berries, fruits, nuts, chocolate, vegetables, and products thereof constitute common foods and beverages with high antioxidant values" (Monica et al., 2010). Herbs and supplements include the most antioxidant-rich products.
3. Get Enough Protein
Protein intake and individual amino acids can affect brain function and mental health. This is due to the neurotransmitters produced from amino acids. Two, in particular, are tryptophan and tyrosine - an essential amino acid that our bodies don't make and a standard amino acid we do make, respectively.
Tryptophan is responsible for making our mood regulating neurotransmitter serotonin while tyrosine makes dopamine - our pleasure neurotransmitter. "Tryptophan consumption has the potential to reduce depressive symptoms and anxiety" (Friedman, 2018). Lack of these nutrients results in low mood and motivation.
4. Help Your Stressed HPA Axis
Your HPA axis is your hypothalamic pituitary adrenal axis. The HPA axis includes a group of hormones from the nervous and endocrine systems: the hypothalamus, pituitary gland, and adrenal glands. The primary function of the HPA axis is to regulate the stress response. When you experience something stressful, your body releases a stress hormone called cortisol. This then causes a number of changes that help the body to deal with stress.
Stress, especially chronic stress that has built up over time, can cause an imbalance in your body affecting your cortisol production and gut balance. With these imbalances, tremendous negative outcomes, such as poor sleeping patterns, poor healing, poor immunity, anxiety, and depression, come with it. "These alterations in the microbiota influence stress-related behaviors" (Foster, 2013). If not managed or treated, anxiety may worsen and often develop into depression and sleeping problems.
Research has confirmed a myriad of health benefits associated with the practice of meditation and decreased anxiety. Meditation is surprisingly useful in reducing stress and anxiety which in turn would regulate your stress response. Meditation continues to grow in popularity in adults and children.
Avoid negative thoughts as "repetitive negative thinking has shown positive and significant associations with symptoms of depression and anxiety" (Rood et al., 2010). There is also a correlation with negative moods increasing inflammation in the gut thus affecting the brain and mood leading to anxiety.
Therapy may be helpful. If it's not affordable to you, practice it. Talk to yourself as if you were your own therapist or how you would talk to your friends and family if they were going through a difficult time. The actions you take will align with your values of self-love. Value yourself. This is a practice that will take time.
Conclusion
As you can see, mental health and nutrition are vital for living life and helping anxiety. It can feel tough. However, when you feel like your anxiety is taking over and there is no other way but to just take medication realize that your anxiety is not taking over your life. We just have to find the root cause. This is why nutrition and learning how to manage stress is so vital to our health, our well-being, and our gut microbiota.
Remember, nutrition is just as important as mental health. Learn to manage stress. It is understood that stress is good in certain aspects as it helps a person with defense mechanisms. However, it is when it becomes chronic that it affects the overall quality of life.
If stress is managed then sleep, immunity, and most importantly, your anxiety may get better! This helps regulate your HPA axis which in turn will make your gut happy and less inflamed. Meditation, avoiding negative thoughts, and therapy may be helpful.
Prioritize your food intake with food that will fuel your gut microbiota and feed it with those nutrient-dense foods that your gut and brain will thank you for later.
Overall, feeding your gut with nutritious foods, providing yourself with self-care, and love to relax your mind and body can provide you with so many benefits for your anxiety. Nutrition and stress management make a huge impact on the gut and its relationship to the brain and behaviors.
If you have issues with your anxiety, please seek out a professional such as your doctor, therapist, and/or dietitian to help guide you through your journey for battling anxiety.
References
Carlsen, M. H., Halvorsen, B. L., Holte, K., Bøhn, S. K., Dragland, S., Sampson, L., ... & Barikmo, I. (2010). The total antioxidant content of more than 3100 foods, beverages, spices, herbs and supplements used worldwide. Nutrition Journal, 9(1), 3.
Clapp, M., Aurora, N., Herrera, L., Bhatia, M., Wilen, E., & Wakefield, S. (2017). Gut microbiota's effect on mental health: the gut-brain axis. Clinics and Practice, 7(4).
Cryan, J. F., & Dinan, T. G. (2012). Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nature Reviews Neuroscience, 13(10), 701-712.
Do, M. H., Lee, E., Oh, M. J., Kim, Y., & Park, H. Y. (2018). High-glucose or-fructose diet cause changes of the gut microbiota and metabolic disorders in mice without body weight change. Nutrients, 10(6), 761.
Dueñas, M., Muñoz-González, I., Cueva, C., Jiménez-Girón, A., Sánchez-Patán, F., Santos-Buelga, C., ... & Bartolomé, B. (2015). A survey of modulation of gut microbiota by dietary polyphenols. BioMed research international, 2015.
Felger, J. C. (2018). Imaging the role of inflammation in mood and anxiety-related disorders. Current Neuropharmacology, 16(5), 533-558.
Foster, J. A., & Neufeld, K. A. M. (2013). Gut-brain axis: how the microbiome influences anxiety and depression. Trends in Neurosciences, 36(5), 305-312.
Friedman, M. (2018). Analysis, nutrition, and health benefits of tryptophan. International Journal of Tryptophan Research, 11, 1178646918802282.
Graham-Engeland, J. E., Sin, N. L., Smyth, J. M., Jones, D. R., Knight, E. L., Sliwinski, M. J., ... & Engeland, C. G. (2018). Negative and positive affect as predictors of inflammation: timing matters. Brain, Behavior, and Immunity, 74, 222-230.
Jena, P. K., Prajapati, B., Mishra, P. K., & Seshadri, S. (2016). Influence of gut microbiota on inflammation and pathogenesis of sugar rich diet induced diabetes. Immunome Research, 12(1), 109-119.
Kiecolt-Glaser, J. K., Belury, M. A., Andridge, R., Malarkey, W. B., & Glaser, R. (2011). Omega-3 supplementation lowers inflammation and anxiety in medical students: a randomized controlled trial. Brain, Behavior, and Immunity, 25(8), 1725-1734.
Miller, M. J., Angeles, F. M., Reuter, B. K., Bobrowski, P., & Sandoval, M. (2001). Dietary antioxidants protect gut epithelial cells from oxidant-induced apoptosis. BMC Complementary and Alternative Medicine, 1(1), 11.
O'Mahony, S. M., Clarke, G., Borre, Y. E., Dinan, T. G., & Cryan, J. F. (2015). Serotonin, tryptophan metabolism and the brain-gut-microbiome axis. Behavioural Brain Research, 277, 32-48.
Rao, T. S., Asha, M. R., Ramesh, B. N., & Rao, K. J. (2008). Understanding nutrition, depression and mental illnesses. Indian Journal of Psychiatry, 50(2), 77.
Rood, L., Roelofs, J., Bögels, S. M., & Alloy, L. B. (2010). Dimensions of negative thinking and the relations with symptoms of depression and anxiety in children and adolescents. Cognitive Therapy and Research, 34(4), 333-342.
Sharma, H. (2015). Meditation: process and effects. Ayu, 36(3), 233.
Xu, Y., Wang, C., J Klabnik, J., & M O'Donnell, J. (2014). Novel therapeutic targets in depression and anxiety: antioxidants as a candidate treatment. Current Neuropharmacology, 12(2), 108-119.
Yano, J. M., Yu, K., Donaldson, G. P., Shastri, G. G., Ann, P., Ma, L., ... & Hsiao, E. Y. (2015). Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell, 161(2), 264-276.
Ease That Itch: Natural Remedies for Eczema
Rachel Wright, Dietetic Intern 2021

Eczema: The Itch has Increased
The prevalence of eczema has increased by about 12% since the 1990’s (National Eczema Association, n.d.). Approximately 31.6 million children and adults suffer from eczema, accounting for roughly 10.1% of the U.S. population. How is it that we haven’t found the cure yet? There is an abundance of research on pharmaceutical treatments used to abate symptoms, but fewer studies covering natural remedies for this disease. Diet and herbal treatments have been used to heal and cure diseases for thousands of years, how can we use those traditions to improve eczema in our population today?
The Scenario
I know how it goes, you have terrible rashes, itching, scaling or redness for weeks, months, maybe even years, and finally your doctor diagnoses you with eczema – only to be given standard treatment options that may alleviate some discomfort. Is that really all you can do? There must be other ways to help without using steroids and creams that have side effects that are equally as uncomfortable as the eczema itself, right? Well you are correct in thinking this, there are other options, and I’m here to help you find them.
My Familial Tie
My brother-in-law has struggled with eczema his entire life. In childhood, his symptoms were not severe and his family didn’t see a need for treatment. It wasn’t until middle school that his eczema was deemed severe enough to seek treatment from a medical professional. At that point, he was told to take the traditional treatment route of steroid creams, which seemed to alleviate his symptoms at the time. Now, well into his twenties, the intensity and frequency of flare-ups are impacting his daily life. He becomes embarrassed by the flare ups making him choose to wear long sleeves on a warm day, say no to outings with coworkers and friends, and feel helpless on what to do. On top of all of that, the constant itch is extremely uncomfortable to live with. He wishes that he had started treatment sooner, had found alternatives to the traditional treatment options, and that he didn’t feel stuck with a disease he doesn’t know how to treat.
A Different Approach
Herbal remedies have been used traditionally for hundreds of years to treat skin conditions. Despite their historic popularity and effectiveness with nearly every disease, they have not been studied nearly as much as you would expect. Still, there is evidence to support the idea that herbal remedies should be considered as additional or alternative treatment to numerous ailments. The top herbal remedies used traditionally for eczema include aloe vera, indian pennywort, walnut, jujube, chamomile, rosemary, liquorice, turmeric and calendula (Khiljee et al, 2011). Some of these remedies are intended for topical use, while others can be ingested orally in order to alleviate eczema symptoms. We will focus on turmeric and indian pennywort. According to research, these two herbs have been found to significantly alleviate common eczema symptoms such as scaling, itching, redness, and skin thickening (Khiljee et al, 2011).
The Golden Root: Turmeric
Turmeric, also known as curcuma longa, is a plant in the ginger family. It is packed with a variety of nutrients and can be recognized by its distinct yellow color. This herbal remedy can be utilized in many forms such as a paste, cream, or gel, and it can be taken orally by adding it to meals or drinks. Turmeric has strong antifungal and antiviral properties and is commonly used to treat wounds and inflamed joints (Chattopadhyay et al, 2004). Topically, this herb has been found in research to decrease symptoms associated with eczema including erythema, scaling, skin thickening, and itching (Vaughn et al, 2016). One thing to note – if you desire to use turmeric topically, it’s important to be aware that it can stain fabrics and surfaces. Orally, this herb has been found in research to alleviate symptoms for a variety of skin conditions. Turmeric is not well absorbed in the body, so you must take it with an absorption enhancer. In research, it has been found that adding black pepper to turmeric can increase its bioavailability by 2000%, allowing it to provide desired health effects in the body (Vaughn et al, 2016 and Hewlings et al, 2017). One method of using this herb orally is to make homemade turmeric milk (Delzell, 2020). Turmeric milk can be made very easily by combining 2 cups unsweetened almond or coconut milk, 1 tbsp agave or honey, 1 tbsp extra virgin coconut oil, 1 tsp ground turmeric, 1 cinnamon stick or 1 tsp ground cinnamon, and a pinch of pepper. The first step is to warm up the milk, once you’ve done this all you need to do is add the remaining ingredients, whisk them together, and strain the liquid. You can drink up to 2 cups of this turmeric milk daily, but should not exceed 8g (or approximately 2 tsp) turmeric per day (Vaughn et al, 2016). Research has found that drinking turmeric can help heal your body from the inside out, alleviating symptoms of eczema without having to use the turmeric topically.
The Power of a Flowering Plant: Indian Pennywort
Indian pennywort, also known as Centella Asiatica, is an herbaceous plant native to Asia. This herb is known for its incredible healing properties (Park et al, 2017 and Kunwar et al, 2005). The plant has strong antioxidant and hydrating properties that provide soothing effects to the skin. Traditionally, it was used in the treatment of leprosy and since then has been found to aid in the treatment of a variety of ailments. You can ingest indian pennywort orally in salads, curries, and teas, or use it topically as a gel or cream (Das, 2011). Indian pennywort is rich in a variety of the B vitamins, vitamin C, and carotenoids, and is commonly consumed in Indonesia to complete a well-balanced diet.
Eczema’s Connection with Food
In addition to traditional herbal remedies, another factor that greatly impacts eczema symptoms is your diet. The food you eat impacts a multitude of things including brain function, gut health, and most pertinently, eczema symptoms. Food allergies or intolerances have been found to intensify eczema symptoms and cause flare ups (Breuer et al, 2004). Common allergenic foods for eczema include cow’s milk, eggs, gluten, and soy. In order to assess whether or not these foods are causing issues for you, it is helpful to speak with your physician about running some tests and completing an elimination diet. With the help of test results and the diet you can narrow down which foods may be problematic for your eczema. Eliminating these allergenic foods – milk, eggs, gluten, and soy, may help to abate your symptoms. It is not recommended to avoid these foods forever though, the goal is to eliminate them for a few weeks and then slowly re-introduce each food, one at a time, a few days apart, to see if your symptoms return after the reintroduction of a certain allergenic food (IFM, 2014). The goal with the elimination diet is to find those trigger foods so you can permanently eliminate them while reintroducing the other items that do not cause you any problems. Your physician will be very helpful during this process, but in addition to their expertise, you can also work with a registered dietitian nutritionist to help you navigate the diet. A dietitian is someone who has received special education and training to best help you find the foods causing problems and how to move forward with your new diet. If you decide not to try the elimination diet, it is important to listen to your body and when flare ups are most severe. Try to notice whether flare ups occur after a certain meal or activity so that you can potentially avoid that trigger in the future. No matter how you decide to address potential allergens, make sure to speak with your doctor before trying something new!
Hista-MEAN: The Impact Histamine Can Have on the Body
Another common cause of worsening eczema symptoms includes the compound histamine (Maintz et al, 2006). Histamine is a chemical produced by the body to defend against allergens such as pollen, mold, and foods (KidsHealth, n.d.). It is an important mediator in itching due to its involvement in the immune response. Research has found that some people impacted by eczema are more sensitive to histamine due to lower diaminoxidase (DAO) activity. Diaminoxidase’s role in the body is to break down excess histamine. Having lower levels of DAO means that the body is not clearing histamine as quickly as it needs to. It has been found that vitamin B6, copper, and zinc have a direct impact on DAO activity (Maintz et al, 2006). When these essential nutrients are deficient or lacking in the body, DAO activity is decreased. For those with histamine intolerance, following a histamine-free diet high in vitamin B6, copper, and zinc would be beneficial in decreasing eczema symptoms. There are many resources on the internet to help understand which foods are high in histamine or those that inhibit DAO activity. One website can be found by searching for: Histamine Intolerance Awareness, check out their resources for further discussion on how to limit histamine containing foods. Similarly, to the elimination diet we discussed above, this diet should not be followed forever and should be done under the care of your physician and registered dietitian.
Eczema is Not Forever
In summary, there are a multitude of remedies for eczema that don’t involve steroids or chemically-created creams, including the two we discussed today – turmeric and indian pennywort. While there is a time and place for standard treatment methods, herbal and dietary remedies are great supplementary methods to further alleviate symptoms. It is important to discuss with your physician before stopping current eczema treatments or trying these dietary recommendations. With the addition of diet changes and herbal remedies– methods that have been used by many past generations to heal their skin– you can ease that itch.
References
Breuer, K., Heratizadeh, A., Wulf, A., Baumann, U., Constien, A., Tetau, D., Kapp, A., Werfel,
T., 2004. Late eczematous reactions to food in children with atopic dermatitis. Clinical & Experimental Allergy, 34(5), 817-824). Retrieved from https://pubmed.ncbi.nlm.nih.gov/15144477/
Chattopadhyay, I., Biswas, K., Bandyopadhyay, U., & Banerjee, R. (2004). Turmeric and
curcumin: Biological actions and medicinal applications. Current Science, 87(1), 44-53. Retrieved from http://www.jstor.org/stable/24107978
Coder, Kim., 1999. Your black walnut tree is out to get you. Retrieved from
https://newswire.caes.uga.edu/story.html?storyid=3629&story=Killer-Tree
Das, Amar Jyoti., 2011. Review on Nutritional, Medicinal and Pharmacological Properties of
Centellaasiatica (Indianpennywort). Journal of Biologically Active Products from Nature. 1(4), 216-228, Retrieved from: https://doi.org/10.1080/22311866.2011.10719089
Delzell, Emily. 2020. Get the Facts: Turmeric. Retrieved from
https://nationaleczema.org/get-the-facts-turmeric/
Hewlings, S. J., & Kalman, D. S. (2017). Curcumin: A Review of Its Effects on Human Health.
Foods (Basel, Switzerland), 6(10), 92. https://doi.org/10.3390/foods6100092
IFM., 2014. Elimination Diet: Comprehensive Guide. Retrieved from
https://experiencelife.lifetime.life/article/the-institute-for-function…
Khiljee, Sonia., Rehman, NU., Khiljee, Tanzila., Ahmad, RS., Khan, MY., Qureshi, UA., 2011.
Use of traditional herbal medicines in the treatment of eczema. J. Pak. Dent. Assoc, 21(2), 112-117. Retrieved from https://www.researchgate.net/publication/291863338_Use_of_traditional_h…
Khiljee, Sonia., Rehman, NU., Khiljee, Tanzila., Loebenberg, Raimar., Ahmad, RS., 2015.
Formulation and clinical evaluation of topical dosage forms of Indian Penny Wort, walnut and turmeric in eczema. Pak J Pharm Sci, Nov 28(6), 2001-7. Retrieved from https://pubmed.ncbi.nlm.nih.gov/26639477/
KidsHealth., n.d. Definition: Histamine. Retrieved from
https://kidshealth.org/en/parents/histamine.html
K-State Research and Extension., 2015. Landscaping near black walnut trees. Retrieved from
https://www.johnson.k-state.edu/docs/lawn-and-garden/in-house-publicati…
Kunwar, R. M., Nepal, B. K., Kshhetri, H. B., Rai, S. K., & Bussmann, R. W. (2006).
Ethnomedicine in Himalaya: a case study from Dolpa, Humla, Jumla and Mustang districts of Nepal. Journal of ethnobiology and ethnomedicine, 2, 27. Retrieved from https://doi.org/10.1186/1746-4269-2-27
Maintz, Laura., Benfadal, Said., Allam, Jean-Pierre., Hagemann, Tobias., Fimmers, Rolf.,
Novak, Natalija., 2006. Evidence for a reduced histamine degradation capacity in a subgroup of patients with atopic eczema. J Allergy Clin Immunol. 117(5), 1106-12. Retrieved from https://pubmed.ncbi.nlm.nih.gov/16675339/
National Eczema Association. (n.d.). Eczema Stats. Retrieved from
https://nationaleczema.org/research/eczema-facts/
Park, J. H., Choi, J. Y., Son, D. J., Park, E. K., Song, M. J., Hellström, M., & Hong, J. T. (2017).
Anti-Inflammatory Effect of Titrated Extract of Centella asiatica in Phthalic Anhydride-Induced Allergic Dermatitis Animal Model. International journal of molecular sciences, 18(4), 738. https://doi.org/10.3390/ijms18040738
Plants for a future., N.d. Centella asiatica. Retrieved from
https://pfaf.org/user/Plant.aspx?LatinName=Centella+asiatica
Vaughn, AR., Branum, Amy., Sivamani, RK., 2016. Effects of turmeric (curcuma longa) on skin
health: a systematic review of the clinical evidence. Phytotherapy Research, 30(8), 1243-1264. Retrieved from https://onlinelibrary.wiley.com/doi/abs/10.1002/ptr.5640
Can Food Fix COPD?
Leslie Rowe, Dietetic Intern 2018

Introduction
Everyone has experienced a conversation when the other person shares a new fact that sounds too good to be true, but your own lack of knowledge on the topic leaves you forced to nod and smile in curiosity. I'm not alone am I? I was stuck in this situation when visiting a patient in a hospital as he exposed me to a diet that reportedly cured chronic obstructive pulmonary disease (COPD). I had never heard of any diet specifically for COPD, so I was intrigued to pick his brain for the details. He raved about how eating a diet low in carbohydrates helped to reduce his respiratory issues and also caused him to lose 36 pounds in 6 months. The book he found his information and diet tips from was titled, "Diet That Began My Mother's Recovery from COPD" by W.G. Miller. For those of you struggling with COPD or have a family member with this disease, I'm sure you are intrigued to read further into my findings after reading this book and digging into research about the possibility of a diet to help with COPD.
Overview of COPD
First, let's dive into a review of what COPD is, the symptoms that occur, and usual medical treatment. COPD is a progressive disease of the lungs, ranging from mild to severe, that is the third leading cause of death in the United States.1 It's caused by long-term exposure to irritating gases or particulate matter, most often from cigarette smoke.2 The disease includes chronic bronchitis and emphysema, and both are characterized by an inflamed airway that decreases the amount of oxygen that flows to your body tissues. Long-term exposures to cigarette smoke, irritating gas, or matter can cause one of the two conditions. The air sacs in the lungs lose the elastic quality and eventually destroy lung tissue in emphysema, and inflammation and an excess of mucus obstructs the airways, which causes shortness of breath in chronic bronchitis. This chronic shortness of breath will eventually limit one's ability to stay active and perform daily activities. Common symptoms with chronic bronchitis are a chronic cough with sputum, but other symptoms of emphysema will worsen over time as lung damage occurs. Common symptoms of COPD are fatigue, chronic cough, wheezing, chest tightness, unintended weight loss, and frequent respiratory infections. Living with this chronic disease can also affect mental health; it's not uncommon to feel fear, anxiety, depression, or stress.3 Accurate diagnosis of COPD includes your doctor reviewing the symptoms, medical history, and environmental exposure as well as pulmonary function tests and X-rays. There is currently no cure for COPD, but it is considered preventable and treatable. Early detection of COPD is vital to maintenance and treatment as well as smoking cessation.4 Effective therapies have been used to reduce symptoms and complications of COPD. Bronchodilators and inhaled steroids may be used in inhalers to relax muscles and reduce inflammation in the airways, or supplemental oxygen during daily activities may be needed. Vaccines and antibiotics are also widely used to treat associated infections in the lungs.
Miller's Book Review
Now that everyone is refreshed on COPD and how this disease affects the body, I want to share with you the contents of the book that first introduced me to a diet to cure COPD. The patient I referred to earlier read the book titled, "Diet That Began My Mother's Recovery from COPD" by W.G. Miller.5 Miller's mother had emphysema, and he was determined to find a way to not only slow the progression of the disease but also cure it completely. As Miller watched her disease progress, he noticed her distending lungs eventually began crowding her stomach little by little as well as an increase in need oxygen required during mealtime, which resulted in a decrease in meal sizes that caused weight loss.5 After researching COPD and current treatments, he believes opportunistic fungi that compromise the body's immune system causes this disease. He found evidence about how disease-like pathogens live off of sugar in the body and hypothesized that if there were no sugar in the diet to provide pathogens a food supply, these pathogens would not be able to survive. Using this hypothesis, Miller developed a diet plan to eliminate simple sugars and grains. As his mother's primary caregiver who prepared all of her meals, he began a two-week transition of elimination of foods like bread, cereal, potatoes, and pasta without her knowledge. He described the subtle improvements just after two weeks, as his mother was no longer gasping for air when walking, her mood overall improved, she was sleeping more, and she was eating! After the diet was in full swing, the basic layout was three meals per day with a snack only occasionally and one "cheat" meal per week. He includes many examples on well-balanced meals for breakfast, lunch, dinner, and snacks, so I included an example of each below:
| Breakfast | Lunch | Dinner | Snack |
|---|---|---|---|
| Scrambled eggs with diced ham and green peppers; one half orange; coffee with powdered cream. | Chicken soup with carrots, white onions and garlic; sliced tomatoes; romaine salad with cherry tomatoes, yellow squash, and white onions; Balsamic vinaigrette dressing. | Garlic and chive marinated, baked pork steaks; steamed fresh peas and carrots with crushed garlic; spinach salad with hard-boiled egg, ham, and white onions; Balsamic vinaigrette dressing; fresh strawberries and cherries. | Cashews |
The diet Miller and his mother followed consisted mainly of uncontaminated protein and fresh vegetables, with plenty of water to drink, milk in moderation, and coffee in the morning. Miller includes many tips to preparing healthy meals, such as herb seasoning to meat and vegetables instead of using condiments, marinating meat before baking, grilling, stir-frying, or using the crock-pot, and consuming either raw or steamed vegetables for variety at each meal. This diet worked long-term for his mother, as she showed great improvement from just implementation of this diet.5 Miller writes other books, one that details supplements that were able to complete his mother's recovery, and another that is a complete guide to her recovery journey with all details inside. I was amazed and glad a diet was able to improve the condition of emphysema in one person but intrigued to find out if research supported this hypothesis by Miller.
Does Research Support the Book?
As I began my search for research on this topic, the main diet-related concern with COPD I noticed was unintentional weight loss and malnourishment. Malnutrition is common in those with COPD due to the combination of appetite loss, decreased physical activity, or depression, which result in decreased dietary intake.6 After digging deeper, the consensus is that the idea of a diet to cure COPD is a new concept that is not well researched at this point. Some research shows a correlation of a Mediterranean style diet with improved lung function, due to the antioxidant benefits extracted from the diet and defense against inflammation and oxidants.7 Since Miller's diet resembles a paleo diet, one with a low amount of processed foods and refined sugars to reduce fungi in the lung microbiota, I focused my findings on these microorganisms.
One study analyzed the variation of bacteria and fungi found in the sputum of patients with COPD, with results showing the microbial communities continuously change during COPD exacerbations and are personalized to each individual. The lung microbiome of these COPD patients was revealed to have varied types of fungi, such as candida, Phialosimplex, and Aspergillus.8 Since symptoms of severe asthma can resemble COPD symptoms, a clinical trial showed 29% of patients had sensitivities to at least 1 fungal allergen, such as Candida or Aspergillus, and multiple sensitizations were associated with poor asthma control.9 With research to support that fungi, specifically Candida, can be present in lung microbiota, this study examined the association of long-term and recent diets with fungal populations within the gut. "Candida [was] positively associated with diets high in carbohydrates, but negatively with diets high in amino acids, protein, and fatty acids."10 Also, a high abundance of Candida was most prevalent after recent consumption of carbohydrates.10
These results give support to Miller's hypothesis and diet plan, but not without a few unanswered questions. Fungi in the gut and vaginal microbiome can be altered by the diet, but is this also true for fungi found in the lungs? One article suggested that since the gut microbiota helps shape the immune system, it does also affect the lung mucosa, but more research is needed.11 Also, I was unable to find research articles specifically looking at a diet high or low in carbohydrates and underlying effect on lung function in those with COPD. Has this theory been researched before or is Miller one of the first to try this diet for COPD? Until more evidence is published, Miller's diet approach remains a hypothesis.
Conclusion
I hope my small amount of research to get to the bottom of a nutrition claim has helped those of you who live with COPD. The diet that helped Miller's mother recover from COPD worked in his favor, but there are currently not enough studies to fully support this diet as a proven intervention. With this in mind, if I had the chance to interact again with the patient who brought this book to my attention, I would support him in following the diet if he believed saw signs of improvement; however, I would ensure he was replacing the calories lost by removing simple carbohydrates from his diet with other nutritious foods and meets an adequate caloric goal each day. I am looking forward to monitoring this topic for further research in the future, as any possibility to treat chronic disease with nutrition is exciting and important for the health of each generation.
References
1. O'Neil, Kevin M. Learn About Chronic Obstructive Pulmonary Disease (COPD). Chest Foundation. https://foundation.chestnet.org/patient-education-resources/copd/ Updated February 2018. Accessed April 15, 2018.
2. Mayo Clinic Staff. COPD. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/copd/symptoms-causes/syc-20353679 Published August 11, 2017. Accessed April 15, 2018.
3. American Lung Association. Chronic Obstructive Pulmonary Disease (COPD). American Lung Association. http://www.lung.org/lung-health-and-diseases/lung-disease-lookup/copd/ Published 2018. Accessed April 15, 2018.
4. National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. Chronic Obstructive Pulmonary Disease (COPD). Centers for Disease Control and Prevention. https://www.cdc.gov/copd/index.html Updated August 4, 2017. Accessed April 15, 2018.
5. Miller, W.G. Diet That Began My Mother's Recovery from COPD. 2012. Accessed April 1, 2018.
6. Seo, SeungHee, Medical Nutrition therapy based on Nutrition Intervention for a Patient with Chronic Obstructive Pulmonary Disease. ClinNutr Res. 2014; 3(2): 150-156. Doi: 10.7762/cnr.2014.3.2.150.
7. Yazdanpanah, Leila, Paknahad, Zamzam, Moosavi, Ali Javad, Maracy, Mohammad Reza, and Zaker, Mohammad Masoud. The relationship between different diet quality indices and severity of airflow obstruction among COPD patients. Med J Islam Repub Iran. 2016; 30: 380. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4972049/ Published May 31, 2016. Accessed April 15, 2018.
8. Su J, Liu H-y, Tan X-l, Ji Y, Jiang Y-x, Prabhakar M, et al. Sputum Bacterial and Fungal Dynamics during Exacerbations of Severe COPD. PLoS ONE 2015; 10(7): e0130736. https://doi.org/10.1371/journal.pone.0130736
9. Masaki K, Fukunaga K, Matsusaka M, Kabata H, Tanosaki T, Mochimaru T, Kamatani T, Ohtsuka K, Baba R, Ueda S, Suzuki Y, Sakamaki F, Oyamada Y, Inoue T, Oguma T, Sayama K, Koh H, Nakamura M, Umeda A, Kamei K, Izuhara K, Asano K, Betsuyaku T. Characteristics of severe asthma with fungal sensitization. Ann Allergy Asthma Immunol. 2017; 119(3): 253-257. Doi: 10.1016/j.anai.2017.07.008
10. Hoffmann C, Dollive S, Grunberg S, Chen J, Li H, Wu GD, et al.A rchaea and Fungi of the Human Gut Microbiome: Correlations with Diet and Bacterial Residents. PLoS ONE. 2013; 8(6): e66019. https://doi.org/10.1371/journal.pone.0066019
11. Segal, Leopoldo N., Blaser, Martin J. A Brave New World: The Lung Microbiota in an Era of Change. Ann AM Thorac Soc. 2014; 11(Suppl 1): S21-S27. Doi: 10.1513/AnnalsATS.201306-189MG
Your Child's Behavior versus Your Child's Gut: Is There a Connection?
Brandi Gouldthorpe, Dietetic Intern 2018

French psychiatrist Phillipe Pinel, stated: "The primary seat of insanity generally is in the region of the stomach and intestines."
Every year further research studies are published trying to answer the question as to what the underlying causes and treatment options are for disorders and diseases ranging from Autistic Spectrum Disorders, Attention Deficit Hyperactivity Disorder (ADHD/ADD), depression, obsessive-compulsive disorder, schizophrenia and bipolar disorder which are becoming more common in children and young adults.
Having a child with a neurological or psychological disorder mentioned above can change your life in many ways. It can be overwhelming for a parent or family member who experience it 24/7 and can make some days harder than others. But what if your child's behavior or social problems could be managed by changing what they eat?
What Is the GAPS Diet?
Before I dive into the GAPS diet, it is important to know a little background regarding how this diet came about.
In the 1950s a doctor by the name of Sidney Haas developed a diet known as the Specific Carbohydrate Diet (SCD) after she found that eating only simple sugars as your carbohydrate source significantly improved severe intestinal disorders in children. Years later Dr. Natasha Campbell-McBride took the SCD and further enhanced it by adding gut healing protocols in hopes of treating her daughter who had learning disabilities -which is where the GAPS diet or Gut and Psychology Syndrome diet was born. The diet is for psychological or neurological disorders said to be linked to intestinal barrier dysfunction.
What Exactly Do I Mean by Intestinal Barrier Dysfunction?
In recent years, many disorders and diseases have been studied in their connection to the gut. There are imbalances in the gut that usually imply dysbiosis. Gut dysbiosis is when there is a lack of healthy or "good" bacteria in your gastrointestinal track. The bacteria in the gut are needed for digesting food, synthesizing vitamins and fighting infections. The beneficial bacteria are essential to the body's ability to function. When dysbiosis in the gut occurs, the "bad" (or opportunist) bacteria breaks the balance and can cause inflammation. This prolonged inflammation from the overgrowth of bad bacteria and cause damage to the intestinal lining which can lead to increased intestinal permeability (leaky gut).1 So, what exactly is leaky gut? Well in the human body, our gut has over 4,000 square feet of surface area which controls what goes in and what gets absorbed into the bloodstream (when working properly). An unhealthy gut can have cracks or openings in the lining which causes partially digested food and toxins to enter the tissues beneath it which can trigger inflammation and change the healthy bacteria that live in our intestines. 2-4Everyone to some degree has leaky gut (that's normal), but people should not have a constant opening in the gut. Some leaky gut has been shown to be linked to genetics while other factors include modern lifestyles such as the American diet (low fiber and high sugar) has had emerging research. Recent research links the role this inflammation can play in the development of common autoimmune disorders (rheumatoid arthritis, type 1 diabetes, psoriasis) and developmental disorders (autism spectrum disorders and ADHD).
What Does the GAPS Diet Have to Do with Intestinal Barrier Dysfunction?
The gut and the brain have bidirectional communication known as the gut-brain axis (the central nervous system and gut microbiota) and there is substantial evidence associated between this connection and gastrointestinal diseases.
Dr.Campbell-McBride has stated that clinical signs of abnormal gut flora have been shown to be present in almost 100% of mothers of children with neurological and psychiatric conditions. The belief is that when a child does not obtain normal balanced gut flora, food is not digested and absorbed properly and over a prolonged period can lead to developing multiple nutritional deficiencies. Common deficiencies recorded in these patients include magnesium, zinc, B vitamins, calcium, selenium, folic acid, omega 3 and 6 and amino acids - all nutrients important for proper development and function of the brain and immune system.
When a person has an unbalanced gut flora from either dysbiosis or leaky gut, the digestive system becomes a source of toxicity to the body. Abnormalities in cell groups and immunoglobulin are found in individuals. Common factors being candida species, the clostridia family, and gluteomorphins or opiates found in gluten and casein which leads to toxins entering the blood-brain barrier causing different neurological and psychiatric symptoms, showing the connection between the gut and the brain.
There is numerous anecdotal evidence of the GAPS diet's role innormalizing dysbiosis while also healing leaky gut. In order to heal the brain, the first step in the GAPS diet is to heal the gut.
Yes, I know that was a lot to take in, it can be overwhelming at first! The gut is just so fascinating though! So now that you have some background information, take a deep breath…now let's get back to the GAPS diet!
How Does the GAPS Diet Work?
The GAPS diet is broken down into stages and works by restricting foods such as all grains, commercial dairy, starchy vegetables, all processed or refined grains, and focusing on easily digestible and nutrient dense foods that repair and heal the gut such as bone broth and fermented foods. The diet introduces foods that are easier for the body to digest and then to harder foods to digest as tolerated. Foods that the GAPS diet usually avoids is grains, cheese, sugar, and fake sweeteners.
The GAPS diet has an introductory diet for individuals with food allergies and intolerances that are designed to help heal and seal the gut lining. Stage one of the GAPS Diet limits you to broths, soups, and some probiotic-rich foods to slowly introduce the new diet. These foods are important in digestion and aid in healing the gut. In stage two the diet continues to add in foods like egg yolks and meat to add in vegetable stews and casseroles. In stage three, you continue with the foods from the previous two stages but now you can add avocados and sweet vegetables. Stage four focuses on grilled and roasted meats as well as adding cold pressed olive oil, juices, and almond bread (any nut or seed can be used). Stage five is the introduction of cooked apples and raw vegetables. More fruit juices are added at this stage. Stage six adds in raw fruit and honey and dried fruits. The supplementation part of the diet is tailored to each individual based on deficiencies in micronutrients or hormones found in lab and blood work.
The GAPS diet also encourages using all-natural cleaning products and personal care products to help lower any toxic loads or irritants.
The GAPS diet is restrictive and can be hard for a child or even an adult to follow. It is easier to begin when a child is younger, but it can still be done at any stage in life. While it may seem like a daunting task at first, there are many resources to help you along the way and may make a world of difference in your life! Here is a link to a GAPS diet support group. http://www.gapsdiet.com/support.html
Take Away
You can find so many success stories and blogs when searching the GAPS diet, but you can also find stories suggesting that the diet does not work - both can be true. There is not a fix-all one diet. If you have a child who suffers from GI problems and disorders mentioned above and has found that conventional use of medications and pills to treat your child does not work, then this diet might be the right fit! Just remember, it never hurts to try!
The father of modern medicine, Hippocrates, noted: "All diseases begin in the gut."
For the full diet and information visit: http://www.gapsdiet.com/
You can also find some recipe ideas in the recipe section of Gut and Psychology Syndrome, Internal Bliss cookbook, and the Heal Your Gut cookbook.
To learn about Gut and Psychology Syndrome, how it develops and how to treat it effectively with a sound nutritional protocol please read Dr. Campbell-McBride's book "Gut and Psychology Syndrome. Natural treatment for autism, ADHD/ADD, dyslexia, dyspraxia, depression, and schizophrenia"
References
1. Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota's effect on mental health: The gut-brain axis. Clinics and Practice. 2017;7(4):987. doi:10.4081/cp.2017.987[M1] .
2. Conlon MA, Bird AR. The Impact of Diet and Lifestyle on Gut Microbiota and Human Health. Nutrients. 2015;7(1):17-44. doi:10.3390/nu7010017.
3. Li Q, Han Y, Dy ABC, Hagerman RJ. The Gut Microbiota and Autism Spectrum Disorders. Frontiers in Cellular Neuroscience. 2017;11:120. doi:10.3389/fncel.2017.00120.
4. Gillberg C. Disorders of empathy: autism and autism spectrum disorders (including childhood onset schizophrenia). Clinical child neuropsychiatry. February 1999:54-111. doi:10.1017/cbo9780511570094.007.
5. Ferrari P et al. Immune status in infantile autism: Correlation between the immune status, autistic symptoms and levels of serotonin. Encephale 14:339-344, 1988.
6. Mu Q, Kirby J, Reilly CM, Luo XM. Leaky Gut As a Danger Signal for Autoimmune Diseases. Frontiers in Immunology. 2017;8:598. doi:10.3389/fimmu.2017.00598.
7. Adams JB, Johansen LJ, Powell LD, Quig D, Rubin RA. Gastrointestinal flora and gastrointestinal status in children with autism - comparisons to typical children and correlation with autism severity. BMC Gastroenterology. 2011;11(1). doi:10.1186/1471-230x-11-22.
8. Cryan JF, O'Mahony SM. The microbiome-gut-brain axis: from bowel to behavior. Neurogastroenterology & Motility. 2011;23(3):187-192. doi:10.1111/j.1365-2982.2010.01664.x.
9. Huebner F, Lieberman K, Rubino R, Wall J. Demonstration of high opioid-like activity in isolated peptides from wheat gluten hydrolysates. Peptides. 1984;5(6):1139-1147. doi:10.1016/0196-9781(84)90180-3.
10. Campos M. Leaky gut: What is it, and what does it mean for you? Harvard Health Blog. https://www.health.harvard.edu/blog/leaky-gut-what-is-it-and-what-does-it-mean-for-you-2017092212451. Published September 21, 2017. Accessed April 2, 2018.
11. Is the GAPS Diet the Cure for Autism and ADD? Institute for Integrative Nutrition. https://www.integrativenutrition.com/blog/2015/05/is-the-gaps-diet-the-cure-for-autism-and-add. Published May 6, 2016. Accessed April 2, 2018.
12. Gut and Psychology Syndrome Nutritional Protocol. International Nutrition, Inc. http://www.gapsdiet.com/. Accessed April 2, 2018.
Lion’s Mane: Functional Food or Faux Pas?
Lisa Walters, Dietetic Intern 2021

Have you ever been walking through your health food store and spotted dried medicinal mush-rooms? Maybe you stopped to look at all the names: Shiitake, Reishi, Chaga, Turkey Tail, Lion’s Mane. You may have checked the prices and decided against buying them. Besides, why would you invest in something you know nothing about? If you’re like me, you may have never thought to look into the research. This was my story until Christmas of 2020 when I was gifted a Lion’s Mane mushroom-growing kit. I had seen it my local health food store but never thought to re-search or try them. I heard they were medicinal, but I never knew if there was any scientific re-search to back up those claims. I decided to do more research upon growing them since I finally had a chance to try them.
Is Lion’s Mane a Cure-All?
If you’re anything like me, you may have never heard of Lion’s Mane mushrooms before, or per-haps know very little about them. According to Friedman (2015), Lion’s Mane (Hericium erina-ceus), also known as Yamabushitake, mushrooms are commonly consumed in Asian countries such as Korea, India, China, and Japan. They are eaten for medicinal and culinary purposes. They are eaten for medicinal purposes because they may be a functional food. A functional food is a food that can provide extra health benefits beyond general health such as reducing the risk of diseases. Regardless of their potential functional properties, they are generally regarded as healthy food due to their wealth of phosphorus, magnesium, potassium, and phenolic com-pounds. They are regarded mainly for their beneficial effects on cognition and brain health; how-ever, research has shown benefits beyond these. Claims of functional properties for Lion’s Mane mushrooms include:
- Neuroprotective
- Antibiotic
- Anti-diabetic
- Anti-carcinogenic
- Anti-fatigue
- Anti-hypertensive
- Anti-hyperlipidemic
- Anti-inflammatory
- Anti-oxidative
- Hepatoprotective
- Nephroprotective
You may be thinking this is an unbelievable amount of claims for just one mushroom. Surprising-ly, there is evidence to back many of these claims; however certain caveats exist. Much of this research is conducted with animal models or has only been tested in a lab at this time. Neverthe-less, the potential benefits are astounding. In this blog, I will be discussing Lion’s Mane’s bene-fits on brain health, mental health, sleep, and diabetes because these are the more common claims made about the mushroom (Friedman, 2015).
Reducing Cognitive Decline
Getting older is just a matter of life. We know that our brain tends to become less sharp once we reach an older age. Some people experience slower thought and short-term memory problems, but some, unfortunately, develop neurogenerative diseases. These include Alzheimer’s disease and dementia. Although Lion’s Mane is not a magic pill, it may reduce cognitive decline in older people whether they have a neurogenerative disease or not. In a lab-controlled setting, Lion’s Mane has been shown to promote nerve growth factor (NGF) which helps regrow damaged nerves (Saitsu et al., 2019; Sabaratnam et al., 2013). It may also reduce cell death. This could in-dicate a lower risk for neurogenerative diseases (Sabaratnam et al., 2013). While this was found in a lab animal model, there have been human trials indicating cognitive benefits.
As far as human trials go, Sabaratnam et al., (2013) found that Japanese men and women be-tween the ages of 50-80 years who had mild cognitive impairment improved their cognitive func-tion after taking 250 mg tablets containing dried Lion’s Mane mushroom powder 3 times daily for 16 weeks. A randomized controlled trial by Saitsu et al. (2019) found that healthy partici-pants significantly improved cognitive function when taking 3.2 g/day Lion’s Mane mushroom powder in comparison with the placebo group after 12 weeks. The test used to compare cognitive function is a test often used to diagnose dementia. Those who took the mushroom powder had better scores than the placebo group (Saitsu et al., 2019).
Alzheimer’s Disease and Erinacine A
Patients with Alzheimer’s disease have been found to have lower nerve growth factor (NGF) leading to loss of neurons, synapses, and cell signaling involved in memory (Li et al., 2020). Be-cause Lion’s Mane can stimulate NGF, it is thought that it may be protective against Alzheimer’s and other neurogenerative diseases. Erinacine A, a compound isolated from Lion’s Mane mush-room, has been shown to contribute to neuron regeneration and revive brain signals responsible for memory. In a human study, they gave participants with mild Alzheimer’s disease 350 mg enriched with 5 mg/g erinacine A isolated from the Lion’s Mane mushroom for 49 weeks. The supplement reduced cognitive decline, increasing independence in those Alzheimer’s patients given the mushroom supplement when compared with the placebo group (Li et al., 2020).
Dumping Depression with Lion’s Mane
While increased NGF may prevent and improve neurogenerative diseases, it may also have anti-depressant effects (Chong et al., 2019). It may cause generation of new nerves and improve connections across the brain that allow us to learn. This may lead to anti-depressant effects. Another way Lion’s Mane mushrooms may have beneficial effects on depression is by helping balance neurotransmitters. In an animal model, Lion’s Mane extract has been shown to restore depleted levels of dopamine, norepinephrine, and serotonin. Many mental health disorders, including de-pression, are associated with low levels of these neurotransmitters. The mushroom extract may help with depression through inflammatory markers as well. TNF-a, a marker of inflammation, and IL-10, a marker of anti-inflammation, are associated with depression. Lion’s Mane extract has been shown to improve depression through decreasing TNF-a and increasing IL-10, effectively reducing inflammation and improving depression symptoms (Chong et al., 2019).
Giving Anxiety the Axe
In a study by Nagano et al. (2010), women received 4 cookies either containing .5 g Lion’s Mane mushroom powder in each cookie or a placebo over a period of 4 weeks. They found significant decreases in depression and anxiety symptoms in those taking the mushroom powder after 4 weeks. Participants who took the mushroom powder reported improved fatigue, concentration, and menopause symptoms (Nagano et al., 2010).
Soothing, Sleeping, and Stress
Lion’s Mane may also have beneficial effects on sleep quality and stress (Okamura et al., 2015). One study found that a Lion’s Mane mushroom supplement taken daily for 4 weeks decreased anxiety and insomnia symptoms in stressed patients. They also found the supplement improved chronic stress, sympathetic nervous system activity, and depression symptoms (Okamura et al., 2015).
Diabetes Control with Antioxidant Power
Lion’s Mane mushrooms are abundant in antioxidants (Chaiyasut et al., 2017). This means they may be helpful in managing metabolic disorders, such as diabetes. The main way this mushroom can manage diabetes is through blood sugar control. Lion’s Mane supplementation has been found to reduce blood sugar and improve insulin levels. It has also been shown to improve fasting blood sugar and sugar tolerance. Not only does this functional mushroom improve blood sugars, but studies show it can improve diabetic neuropathy pain through increased antioxidant enzyme activity. Possibly due to the high levels of antioxidants and antioxidant enzymes, Lion’s Mane may also reduce inflammation, further improving diabetes outcomes (Chaiyasut et al., 2017).
Where Can I Find Them?
Now that you’ve heard about the benefits of this functional mushroom, you may be asking your-self where you can get them. Fresh and dried Lion’s Mane are often located at your Asian grocery store, health food store, or even farmers market (“Lion’s Mane Mushrooms: A Brain Booster That Tastes Like Crab Meat,” 2019). Dried Lion’s Mane can be found whole, dried, powdered, mixed in teas, or in supplement form. If you enjoy the growing process, some companies sell growing kits online such as the one I grew. Growing them is as easy as cutting holes in a bag and misting it with water for a couple of weeks. I found the growing process to be very easy and re-warding. Like any mushroom, Lion’s Mane grows wild and may be found on sick and dying trees in cool damp areas. There aren’t any poisonous mushrooms that look similar to it, so it may be an easier mushroom to identify and forage. As with any foraging, it is important to do your research beforehand and understand the risks involved. Always exercise extreme caution and forage at your own risk (“Lion’s Mane Mushrooms: A Brain Booster That Tastes Like Crab Meat,” 2019).
How Do I Use Them?
Since Lion’s Mane is also a culinary mushroom, it can be cooked fresh and eaten (“Lion’s Mane Mushrooms: A Brain Booster That Tastes Like Crab Meat,” 2019). The cooked mushroom has a taste and texture similar to crab or lobster. One way to prepare them is cutting them into “steaks” and pan-frying them with spices until golden brown. Fresh mushrooms can also be dehydrated into a powder. The powder can be used as a seasoning in sauces and soups. The powder can also be steeped to make a mushroom tea (“Lion’s Mane Mushrooms: A Brain Booster That Tastes Like Crab Meat,” 2019).
Conclusion:
All in all, Lion’s Mane mushrooms can be a delicious and easy addition to meals with potential added health benefits. While much research about the functional properties of these mushrooms are done with supplements or in animals, they are a proven healthy food—chock-full of vitamins and nutrients including phosphorus, magnesium, potassium, and phenolic compounds (Friedman, 2015). Research has found cognitive benefits including protection from neurogenerative diseases and reduction of anxiety and depression symptoms in humans. No one food is a cure-all, but in tandem with a balanced diet, Lion’s Mane can add nutrients to any meal with some significant potential health benefits. (Friedman, 2015).
References
Chaiyasut, C., Sundaram, B., & Sivamaruthi, S. (2017). Anti-hyperglycemic property of Hericium erinaceus - a mini review. Asian Pacific Journal of Tropical Biomedicine, 7(11), 1036-1040. https://doi.org/10.1016/j.apjtb.2017.09.024
Chong, P. S., Fung, M. L., Wong, K. H., & Lim, L. W. (2019). Therapeutic potential of Hericium erinaceus depressive disorder. International Journal of Molecular Sciences, 21(163), 1-18. doi:10.3390/ijms21010163
Friedman, M. (2015). Chemistry, nutrition, and health-promoting properties of Hericium erinaceus (Lion’s Mane) mushroom fruiting bodies and mycelia and their bioactive com-pounds. J Agric Food Chem, 63, 7108-7123. DOI: 10.1021/acs.jafc.5b02914
Li, I. C., Chang, H. H., Lin, C. H., Chen, W. P., Lu, T. H., Lee, L. Y., Chen, Y. W., Chen, Y. P., Chen, C. C., & Lin, D. P. C. (2020). Prevention of early Alzheimer’s disease by Erinacine A-enriched Hericium erinaceus mycelia pilot double-blind placebo-controlled study. Frontiers in Aging Neuroscience, 12(155), 1-13. doi: 10.3389/fnagi.2020.00155
Lion’s Mane mushrooms: A brain booster that tastes like crab meat. (2019, November 22). Ty-rantfarms. Retrieved May 2, 2021, from https://www.tyrantfarms.com/lions-mane-mushroom-hericium-erinaceus-grow…
Nagano, M., Shimizu, K., Kondo, R., Hayashi, C., Sato, D., Kitagawa, K., & Ohnuki, K. (2010). Reduction of depression and anxiety by 4 weeks Hericium erinaceus intake. Biomedical Research, 31(4), 231-237.
Okamura, H., Anno, N., Tsuda, A., Inokuchi, T., Uchimura, N., & Inanaga, K. (2015). The effects of Hericium erinaceus (Amyloban 3399) on sleep quality and subjective well-being among female undergraduate students: A pilot study. Personalized Medicine Universe, 4, 76-78. http://dx.doi.org/10.1016/j.pmu.2015.03.006
Sabaratnam, V., Kah-Hui, W., Naidu, M., & David, P. R. (2013). Neuronal Health - can culinary and medicinal mushrooms help? Journal of Traditional and Complementary Medicine, 3(1), 62-68.
Saitsu, Y., Nishide, A., Kikushima, K., Shimizu, K., & Ohnuki, K. (2019). Improvement of cognitive functions by oral intake of Hericium erinaceus. Biomedical Research, 40(4), 125-131.
Should You Avoid High Fructose Corn Syrup in Your Child's Diet?
Tammy Proctor, Dietetic Intern 2018

One of the most concerning topics for a parent is what you will feed your child. According to Psychology Today, 57% of parents are concerned about unhealthy eating. The food we put in our bodies is important, which is why what your child eats and drinks is a legitimate concern. I think it's safe to say, we have all heard that we should either cut back or stop consuming sodas and processed foods.
The CDC reports that 49% of adults and 63% of youth drink at least one sugar-sweetened beverage per day.2 It's been estimated that 61% of the average American diet is made up of highly processed foods.3 One of the main ingredients in these items is high fructose corn syrup (HFCS), which in many cases it is the first ingredient. The dangers of HFCS have been discussed in the news, social media, and many other publications but the question is whether it's really harmful or not. Let's get to the facts!
What Is High Fructose Corn Syrup (HFCS)?
HFCS first began to be used in the 1970s when the cost of sugar was high and corn prices were very low and have continued to be utilized due to the low cost and functionality.4 It's made from corn starch in which the manufacturers use an enzymatic process where the molecules are altered changing some of the glucose into fructose.
As a comparison, the sucrose molecule (table sugar), has a 1:1 ratio of fructose to glucose. There are two main forms of HFCS which are referred to as HFCS 42 and HFCS 55. This indicates the percentage of the molecule that is made up of fructose, so HFCS 42 contains 42% fructose and HFCS 55 has 55% fructose. The remainder of the molecule contains glucose and water.
HFCS 42 is mainly used in manufacturing processed foods and HFCS 55 is predominantly used in sodas.5 So why do they use HFCS? The purpose of using HFCS is to provide sweetness, enhance flavors, reduce water content, reduce freezer burn, enhanced texture and moisture of baked goods, give body and texture in beverages, and it causes the enzymatic browning of baked goods.6
How Is HFCS Metabolized?
Fructose from sugar or HFCS meets the same fate. It arrives in the gut and then is sent directly to the liver. There is a difference between the way glucose and fructose are metabolized. Once glucose reaches the liver it is then either stored as glycogen (for use as energy in the muscle), stored as fat (once glycogen stores are full) or transported to cells for use as energy. Fructose, on the other hand, can only be metabolized in the liver. It is either converted to glucose or when excess is consumed, stored as fat within the liver.
Since fructose metabolism only occurs in the liver, lipogenesis is able to occur more efficiently than with glucose.7 Lipogenesis is the metabolic process in which energy is changed into fat and stored. De novo lipogenesis (DNL) is another form of lipogenesis that may occur where excess carbohydrates are stored as fat and have been shown to occur with excessive consumption of HFCS. Some of the harmful effects that are associated with DNL include elevated triglycerides and fat storage in the liver.8 This is a fancy way of saying that this is the process in which fatty liver disease occurs.
You may be thinking, fruit contains fructose, so should I be concerned with my child eating fruit? Absolutely not! Fruit is full of important vitamins and minerals and is a great addition to any diet. The difference between HFCS and fructose in fruit is the concentration. Fructose that comes from HFCS is a concentrated amount of fructose causing a greater consumption of fructose in products containing HFCS compared to fruit. A large apple has approximately 23 grams of sugar and 13 grams is from fructose. While a 16 oz. bottle of Coke has 52 grams of sugar and 30 grams come from fructose. This is a considerable difference! Not to mention that the apple contains fiber which helps to slow the digestion causing the fructose to make it to the liver at a more gradual pace.9
Common Myths About HFCS
Many of us have preconceived notions about HFCS and may have assumptions that are incorrect so let's clear up some of the myths about high fructose corn syrup.
- HFCS causes obesity -- We can't blame the obesity epidemic on HFCS. There is no one specific cause of obesity, there are many causes; genetics, lack of physical activity, food choices, portion sizes, and many more. The blame cannot be attributed to one specific ingredient in a food item or beverage.10
- HFCS is sweeter than sucrose -- Many people have the misconception that HFCS is sweeter than sucrose, but it's not. In order to determine how sweet a sweetener is, whether it is artificial or natural, the standard is sucrose. When compared they are equal in sweetness.11 As a matter of fact, the industry produced HFCS as a replacement for sucrose. They are interchangeable, HFCS just has some added benefits such as preservation and increased moisture.
- HFCS is higher in calories than sucrose -- People often think that HFCS has a higher caloric value than sucrose, however, they have the same caloric value in which they both contain 4 kcal/g.12
What Is Concerning About HFCS?
The research on HFCS is conflicting. Some research shows that HFCS is no different than sucrose and other research that shows HFCS has specific effects on the body. The following research is concentrated on adults 18 to 70 and shows some of the negative effects of HFCS:
- Fructose ratios may be higher in some beverages than thought -- In a study by Walker, Dumke, & Goran, they found that certain beverages contained 60% fructose, which is contradictory to the 55% that they were thought to have contained. This shows that fructose consumption may be more than previously thought due to the increased percentage of fructose in the ratio of the HFCS that was used.13
- Excessive consumption of HFCS may lead to non-alcoholic fatty liver disease (NAFLD) -- An animal study evaluating the effects of HFCS 55 showed that rats who consumed sugar solutions had increased total food intakes when compared to rats drinking water. When the study concluded there was no change in body weight gain but when the rats were dissected it was found they had higher liver weight, total liver, and triglyceride content than the rats who drank water. These findings are alarming because the excess weight of the liver indicates that there was lipid accumulation suggesting that de novo lipogenesis occurred. Ultimately, the study determined that the type of excess sugar does influence hepatic lipid metabolism and influences the advancement of NAFLD, therefore it is advisable to limit the consumption of HFCS and sweetened beverages containing calories.14
- Consumption of HFCS may increase the risk of cardiovascular disease (CVD) -- A study published in the American Journal of Clinical Nutrition, revealed that the consumption of beverages including 10%, 17.5%, or 25% of HFCS showed to have a relation to increased risk of CVD. The results displayed that HFCS increased 6 biochemical markers which can increase CVD mortality risk.15
- Role of HFCS in metabolic syndrome and lipogenesis -- Metabolic syndrome is made up of a group of conditions including elevated blood pressure, high blood sugar, excess abdominal fat, and high cholesterol or triglyceride levels. These conditions increase the risk for heart disease, stroke, and diabetes. The intake of fructose has been linked to increased levels of triglyceride synthesis and lipogenesis in the liver and may contribute to visceral adiposity causing metabolic alterations to occur, leading to insulin resistance. Insulin resistance is when cells no longer properly respond to insulin making it difficult for glucose to get inside the cells. The pancreas continues to try to produce insulin because blood glucose levels are elevated and can eventually lead to type 2 diabetes due to the body's inability to regulate blood glucose levels.16
A study by Stanhope et al., comparing sugar-sweetened beverages that contained glucose or fructose, showed that weight gain was similar amongst both groups; however, there were significant increases in visceral adiposity (fat stored in the abdomen) in the fructose group.17 The evidence shows that visceral adiposity is one of the causation factors of metabolic syndrome.18 Furthermore, a study by Hu & Malik containing 6,000 adult subjects showed a 39% increased risk for metabolic syndrome when subjects consumed one or more soft drinks per day over four years.19
Suggestions to Cut Out HFCS and Added Sugar
Looking at all the facts, the reality about HFCS is it carries all the risks of sucrose plus potentially other risks previously mentioned that most parents would want to avoid in feeding their children. HFCS, whether it is or isn't thought of as the worst ingredient in many foods and beverages, it is still considered added sugar. The American Academy of Nutrition and Dietetics recommends no more than 10% of your daily caloric intake should come from added sugar. This equates to approximately 12 teaspoons or 48 g of sugar per day.20 A typical breakfast for a child may include Cap N' Crunch cereal. If a child consumed ¾ of a cup, it would contain 12 grams of sugar, which is equal to 3 teaspoons of sugar in just the cereal alone.21 Depending on the appetite or size of the child, this could be double or triple that amount in just one meal. Being vigilant in watching how much HFCS or added sugar your child is consuming is one of the main ways you can be assured your child is not getting excessive amounts of added sugar and forming habits that will increase their risk for chronic diseases and/or obesity. Here are a few tips for parents to decrease or cut HFCS or added sugar from their child's diet:
- Reading your food labels -- HFCS and added sugar are in many of the foods we purchase at the grocery store including:
| Beverages | Condiments |
| Cereals | Granola |
| Candy | Instant oatmeal |
| Chocolate | Frozen foods |
| Yogurt | Protein/cereal/granola bars |
| Baked goods | Pasta sauce |
| BBQ sauce | Dried/canned fruit |
| Ketchup | Juice |
| Salad dressing | Baby food |
- ConclusionCooking at home -- This allows you to control the ingredients that are being used and decrease the amount of sugar that goes into a recipe.
- Sweeten items with natural sources of sugar by using fruit -- An example would be using unsweetened oatmeal and adding fruit to give it that sweetened flavor or adding fruit in water to improve flavor.
- Lead by example -- Children learn their eating habits from the way their parents eat. How you eat, is most likely how your child will eat.
Added sugars, whether sucrose or HFCS, when eaten in excess is a future ticking time bomb for our children's health. There is still not enough evidence to conclusively state that HFCS is any worse than sucrose, however, some of the research shows that HFCS could pose serious health risks when consumed in excess. I'm not trying to vilify HFCS, but rather give parents a better understanding of the risks that accompany the excessive consumption of items that may include this ingredient.
What we do know is that excess intake of any type of sugar regardless of the type has been linked to many chronic diseases and obesity. Parents want what is best for their children, and setting them up with healthy eating habits is an important aspect of how they will eat for the rest of their lives. Limiting the amount of excess sugar should be something everyone should be aware of by focusing on limiting the amount we consume. So much of the food we purchase from the grocery store is processed with unwholesome ingredients and full of hidden sugar. I encourage you to look at food labels and pay close attention to what your child is eating because after all, their health is depending on it!
References
1. Top 10 Concerns Parents Have for Their Own Kids (and Others). Psychology Today. https://www.psychologytoday.com/us/blog/the-athletes-way/201708/top-10-concerns-parents-have-their-own-kids-and-others. Accessed April 16, 2018.
2. Nutrition. Centers for Disease Control and Prevention. https://www.cdc.gov/nutrition/data-statistics/sugar-sweetened-beverages-intake.html. Published April 7, 2017. Accessed March 13, 2018.
3. Jennifer M Poti, Michelle A Mendez, Shu Wen Ng, Barry M Popkin; Is the degree of food processing and convenience linked with the nutritional quality of foods purchased by US households?, The American Journal of Clinical Nutrition, Volume 101, Issue 6, 1 June 2015, Pages 1251-1262, https://doi.org/10.3945/ajcn.114.100925
4. Gropper S, Smith J. Advanced Nutrition and Human Metabolism. Cengage Learning, Inc; 2013.
5. Food Additives & Ingredients - High Fructose Corn Syrup Questions and Answers. U S Food and Drug Administration Home Page.
https://www.fda.gov/Food/IngredientsPackagingLabeling/FoodAdditivesIngr…. Accessed March 13, 2018.
6. Fast Facts about High-Fructose Corn Syrup. FoodInsight.org. http://www.foodinsight.org/Fast_Facts_about_High_Fructose_Corn_Syrup. Accessed March 15, 2018.
7. Ter Horst KW, Serlie MJ. Fructose Consumption, Lipogenesis, and Non-Alcoholic Fatty Liver Disease. Nutrients. 2017;9(9):981. doi:10.3390/nu9090981.
8. Adipose tissue de novo lipogenesis. http://www.asbmb.org/asbmbtoday/asbmbtoday_article.aspx?id=15872. Accessed March 17, 2018.
9. Gunnars K. Is Fruit Good or Bad For Your Health? The Sweet Truth. Healthline. https://www.healthline.com/nutrition/is-fruit-good-or-bad-for-your-health. Accessed April 24, 2018.
10. itch C, Keim KS. Position of the Academy of Nutrition and Dietetics: Use of Nutritive and Nonnutritive Sweeteners. Journal of the Academy of Nutrition and Dietetics. 2012;112(5):739-758. doi:10.1016/j.jand.2012.03.009.
11. About High Fructose Corn Syrup. Go to Corn Refiners Association. https://corn.org/products/sweeteners/high-fructose-corn-syrup/. Accessed March 16, 2018.
12. White JS. Straight talk about high-fructose corn syrup: what it is and what it ain't. The American Journal of Clinical Nutrition. 2008;88(6). doi:10.3945/ajcn.2008.25825b.
13. Walker RW, Dumke KA, Goran MI. Fructose content in popular beverages made with and without high-fructose corn syrup. Nutrition. 2014;30(7-8):928-935. doi:10.1016/j.nut.2014.04.003.
14. Mock K, Lateef S, Benedito VA, Tou JC. High-fructose corn syrup-55 consumption alters hepatic lipid metabolism and promotes triglyceride accumulation. The Journal of Nutritional Biochemistry. 2017;39:32-39. doi:10.1016/j.jnutbio.2016.09.010.
15. Stanhope KL, Medici V, Bremer AA, et al. A dose-response study of consuming high-fructose corn syrup-sweetened beverages on lipid/lipoprotein risk factors for cardiovascular disease in young adults. The American Journal of Clinical Nutrition. 2015;101(6):1144-1154. doi:10.3945/ajcn.114.100461.
16. Prediabetes & Insulin Resistance. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance. Published August 1, 2009. Accessed April 16, 2018.
17. Stanhope KL, Schwarz JM, Keim NL, et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. The Journal of Clinical Investigation. 2009;119(5):1322-1334. doi:10.1172/JCI37385.
18. Wajchenberg BL. Subcutaneous and Visceral Adipose Tissue: Their Relation to the Metabolic Syndrome. Endocrine Reviews. 2000;21(6):697-738. doi:10.1210/er.21.6.697.
19. Hu FB, Malik VS. Sugar-sweetened beverages and risk of obesity and type 2 diabetes: Epidemiologic evidence. Physiology & behavior. 2010;100(1):47-54. doi:10.1016/j.physbeh.2010.01.036.
20. Looking to Reduce Your Family's Intake of Added Sugars? Here's How. Eat Right. Academy of Nutrition and Dietetics. https://www.eatright.org/food/nutrition/dietary-guidelines-and-myplate/looking-to-reduce-your-familys-added-sugar-intake-heres-how. Published December 6, 2016. Accessed March 15, 2018.
21. Quaker Oats Company. Cap'n Crunch - Reclaim Your Crunch Time! Cap'n Crunch! http://www.capncrunch.com/. Accessed April 24, 2018.
Is Stevia Better than Other Artificial Sweeteners?
Katie Shumate, Dietetic Intern 2017

Have you heard of stevia? It's an increasingly common zero calorie sweetener that's gained popularity in recent years being praised as the "healthy" and "all-natural" sweetener. Other sweeteners have been linked to increased genotoxicity, cancer (Yilmaz & Ucar, 2014) insulin resistance, metabolic disease as well issues with gut bacteria and other negative side effects (Suez et al., 2014). You've probably seen stevia on the shelves with the yellow, blue and pink sweeteners, but is it really better than the other sweeteners?
I'd like to go over what stevia is, some of its history, how it is extracted and what research has shown about it so we can draw some conclusions about using it.
What Is Stevia?
Stevia is a non-caloric sweeter that is typically sold in either a powder or liquid form that is 200-300 times sweeter than table sugar (Engber, 2014). It has become very popular with the food industry who are trying to find ways to please health conscious customers.
Stevia is made from the leaves of the Stevia rebaudian Bertoni, which is a native shrub in South America, most commonly found in Brazil and Paraguay (Examine.com, n.d.).

There are several chemical compounds that give the plant its sweetness, but the two most abundant and commonly used are stevioside and rebaudioside-A (Stevia.com, n.d). Both of these compounds are steviolglycosides -- a fancy chemical word for a sugar group attached to another chemical functional group. Humans are unable to metabolize the chemical structures of stevioside and rebaudioside-A, giving it the intended sweetness everyone is looking for without the calories. Once stevia reaches the colon, gut bacteria convert steviol glycosides into steviol, which is metabolized by the liver then excreted in the urine (Nichols, 2016). I'll talk more about these two compounds later.
| Stevioside | Rebaudioside-A |
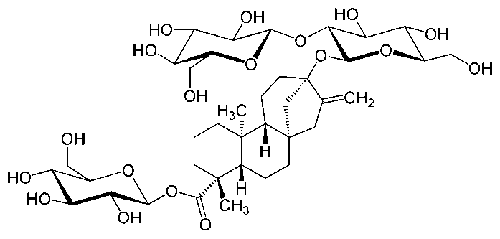 |
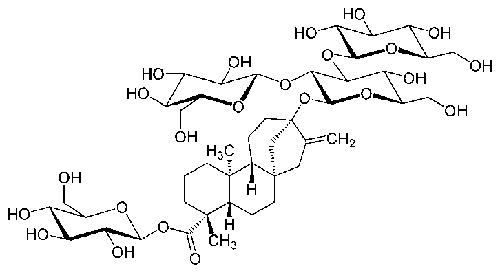 |
Brief History of Stevia
Historically it was used by the Guarani Indians in Brazil. They called it "kaa he he" which means sweet herb. They used it in medicines, in tea, or just to chew on.
In 1887, it was "re-discovered" by Dr. Moises Santiago Bertoni, an Italian college professor. He "found" the stevia plant and made it more well-known to the developed world.
Stevia was presented to the USDA by George S. Brady in 1921 as a new sweetener, but met a lot of resistance in starting up widespread use and manufacturing from the sugar cane companies (Gates, 2000)
In 1931, French scientists isolated the compound stevioside and attributed it to what made stevia taste sweet.
In the 1960s and 1970s, Japan did extensive research on stevia. There was a huge push during this time to eliminate unnatural chemicals in foods, and as a result many things like other artificial sweeteners were banned. A lot of money and research that has continued today was poured into finding a more natural product. By 1988, stevia represented 41% of Japan's non-sugar sweetener market.
In the mid-1980s, stevia became popular in manufacturing and processed goods (Gates, 2000).
Stevia was banned briefly in the United States in 1991 because some animal and cell studies found that it potentially damaged cells and caused cancer. Later studies could not replicate these outcomes and the concentration used in the earlier studies could never be consumed by a human, making the early studies not completely applicable to human health. (Goyal, Samsher, & Goyal, 2010). Other early studies indicated that it may negatively impact the endocrine system and alter hormones, especially in males. Again, later studies could not replicate this outcome and again mentioned the very high concentration of stevioside was not representative of the intake normally consumed in the average human diet (Goyal, Samsher, Goyal, 2010; Oliveira-Filho, Uehara, Minetti, & Valle, 1989).
After much disagreement in the research through the 1990s and early 2000s, finally the compound rebaudioside A gained GRAS or Generally Recognized as Safe status from the Food and Drug Administration (FDA) in 2008 (Stevia.com, 2016). GRAS status is a designation which means that this compound is considered safe by "qualified experts, as having been adequately shown to be safe under the conditions of its intended use" (U.S. Food and Drug Administration, 2017).
In 2008-2009 larger companies like Pepsi, Cargill, and Coca-Cola made their own stevia products (Stevia.com, 2016).
Today there are a ton of stevia products on the shelves!

Forms of Stevia
I told you I would come back to this! So as I said above, rebaudioside-A is the chemical compound approved by the FDA (Examine.com, n.d.). This means it can be sold as a food item (sweetener powder and liquid drops in the regular sweetener isle) and as an additive in things like drinks, candies, and other processed food items. It has a less bitter aftertaste, but has not been studied as extensively as stevioside.
The other structure found in stevia, stevioside, does not yet have approval by the FDA. You can, however, find stevioside at the grocery store! Instead of being in the sweetener isle, stevioside is found in the supplement isle and sold as a medicinal product/sweetener (Examine.com, n.d.). It can be used like a sweetener for your coffee and tea, but it can also be taken like a supplement. Companies are able to do this because supplements are not considered food or drugs and therefore are not evaluated or regulated by the FDA. This can cause some concern over purity and safety. If you would like to use stevioside as a sweetener, I would recommend going with higher quality brands that list stevioside as the only ingredient, often found in drops. It is a little more bitter than rebaudioside, but several studies have found that stevioside has positive health effects.
There is also of course green leaf stevia or whole leaf stevia which is basically whole stevia leaves that have been dried and ground into a powder. It is more bitter than both of the above compounds, but is still 30-40 times sweeter than sugar (Gelski, 2010). I would consider this to be the most natural form of stevia, if that is your concern.
How Is Stevia Extracted?
The extraction process performed by different companies may differ slightly, but they all generally have a multi-step chemical extraction and purification. The liquid and powder form of stevia (rebaudioside-A in the sweetener isle) is made by first drying and grinding up plant leaf cuttings. The leaves are then steeped in hot water (Stevia.com, 2016). The solution then goes through several stages of filtering, centrifuging, and extracting using solvents like acetone, methanol, ethanol, isoproponal and other chemical products (Pasquel, Meireles, Marques, &Ptenate, 2000). Many of these solvents are carcinogenic, and concerns about these harmful solvents remain as it is next to impossible to get rid of all residues (Truth in Advertising, 2014). Food grade stevia has to be at least 95% steviol glycosides to be sold (Stevia.com, 2016). The rebaudioside-A is bottled if it is to become the liquid form,or dried and cut with bulking agents like inulin, maltodextrin, dextrose, or erythritol if made into the powder form. There are also concerns about the bulking agents used. For example, erythritol is a yeast-produced no-calorie sugar alcohol, that may be fed sugars from GMO corn (Engber, 2014).Though stevia originates from a plant, the extraction process may not be as "natural" as we thought.
Current Research
Did you know that stevia isn't just for making your favorite food taste sweeter? There are actual research studies that have found that stevia may be helpful to treat certain health conditions. An animal study done on rats may show that stevia is helpful in the treatment of diabetes. Scientists took a group of rats and gave them diabetes then treated them with stevia extract in their water. They found that though stevia extract did not increase the number of insulin-making beta cells in the pancreas, it helped the rats better use the insulin available by lowering inflammatory chemicals produced by fat cells.
This study showed that steviols have the potential to be a drug treatment for humans in the future, though more research is needed (Akbarzadeh et al., 2014). A study done on humans found that supplementing with stevia in those with type 2 diabetes reduced postprandial blood glucose and glucagon response after a test meal of stevia vs placebo, though other studies have found that stevia supplementation has no significant effects on diabetes. Another study found that stevia may also help lower glucose and insulin levels in those that are not diagnosed with diabetes (Fitch, Keim, Academy of, & Dietetics, 2012).
Other studies showed that stevioside has a positive effect on health by helping to lower blood pressure. In one study, 168 men and women with mild hypertension took 500 mg of stevioside powder or a placebo 3 time a day. After 2 years, the stevioside group had significantly lowered their mean systolic and diastolic blood pressure to a normal range (Hsieh, 2003). Other studies found that stevia had no effect, though all were done for shorter periods of time.
Other studies have shown that stevia extracts alone as well as when they are incorporated into foods act as good antioxidants (Hajihashemi & Ehsanpour, 2014; Ruiz-Ruiz, Moguel-Ordonez, Matus-Basto, & Segura-Campos, 2015).
Many of these studies used stevioside alone or mixtures of stevioside and rebaudioside-A, in much higher doses than you would put in your coffee or tea. No adverse events or issues with safety were reported during these studies. Though more research about long-term use of rebaudioside-A by itself in amounts found in foods, beverages, and added sweeteners should be done, it seem that there is little risk associated with using stevia, especially if you opted to get the stevioside drops found in the supplement isle.
Future Research
There are other glycosides in stevia leaves that have the potential to be just as sweet and useful to the food industry. Companies are now researching rebaudioside-D and rebaudioside-X as possible additives in the future (Gelski, 2010).
Food companies are also researching how to genetically modify yeast to produce the desired glycoside. This would allow companies to produce stevia without the cost of maintaining plants, harvest, cutting, dissolving and heavy processing (Gelski, 2010). The concerns of GMOs will definitely still be present, however.
More research will also be done in the area of long-term use safety and how it affects gut microbiota since this is such a large concern with other artificial sweeteners.
Conclusion
While there are concerns about the chemical residues from the extraction process and added ingredients, it seems that stevia has not been shown to be dangerous, and may even have some health benefits. If you are interested in purchasing stevia for use as a sweetener, I would look for companies that are transparent about processing techniques and for products with the least amount of added ingredients.
References
Akbarzadeh, S., Eskandari, F., Tangestani, H., Bagherinejad, S. T., Bargahi, A., Bazzi, P., . . . Rahbar, A. R. (2014). The Effect of Stevia Rebaudiana on Serum Omentin and Visfatin Level in STZ-Induced Diabetic Rats. Journal of Dietary Supplements, 12(1), 11-22. doi:10.3109/19390211.2014.901999
Engber, D. (2014). The quest for a natural sugar substitute. The New York Times. Retrieved from: https://www.nytimes.com/2014/01/05/magazine/the-quest-for-a-natural-sugar-substitute.html?_r=0G\
Examine.com. Stevia. Retrieved from: https://examine.com/supplements/stevia/
Fitch, C., Keim, K. S., Academy of, N., & Dietetics. (2012). Position of the Academy of Nutrition and Dietetics: use of nutritive and nonnutritive sweeteners. J Acad Nutr Diet, 112(5), 739-758. doi:10.1016/j.jand.2012.03.009
Gates, D. (2000) History of Use. Stevia.net. Retrieved from: http://www.stevia.net/history.htm
Gelski, J. (2010). Stevia needs a baking partner. Food Business News. Retrieved from: http://www.foodbusinessnews.net/News/News-Home/Features/2010/7/Stevia-needs-a-partner-in-baking.aspx?cck=1
Goyal S, Samsher, Goyal R. (2010). Stevia (Stevia rebaudian) a bio-sweetener: a review. International Journal Of Food Sciences And Nutrition. 61(1), 1-10.
Hajihashemi, S., & Ehsanpour, A. A. (2014). Antioxidant response of Stevia rebaudiana B. to polyethylene glycol and paclobutrazol treatments under in vitro culture. Appl Biochem Biotechnol, 172(8), 4038-4052. doi:10.1007/s12010-014-0791-8
Hsieh, M., et. al. (2003). Efficacy and tolerability of oral stevioside in patients with mild essential hypertension: A two-year, randomized, placebo-controlled study. Clinical Therapeutics, 25(11), 2797-2808
Nichols, H. Stevia: Health Benefits, Facts, Safety. Medical News Today. Retrieved from: http://www.medicalnewstoday.com/articles/287251.php
Oliveira-Filho, R., Uehara, O., Minetti, C., & Valle, L. (1989). Chronic administration of aqueous extract of Stevia rebaudiana (Bert.) Bertoni in rats: Endocrine effects. General pharmacology, 20(2), 187-191.
Pasquel, A., Meireles, M.A.A., Marques, M.O.M., & Petenate, A.J.. (2000). Extraction of stevia glycosides with CO2 + water, CO2 + ethanol, and CO2 + water + ethanol. Brazilian Journal of Chemical Engineering, 17(3), 271-282. https://dx.doi.org/10.1590/S0104-66322000000300003
Ruiz-Ruiz, J. C., Moguel-Ordonez, Y. B., Matus-Basto, A. J., & Segura-Campos, M. R. (2015). Nutritional, amylolytic enzymes inhibition and antioxidant properties of bread incorporated with Stevia rebaudiana. Int J Food Sci Nutr, 66(6), 649-656. doi:10.3109/09637486.2015.107778
Suez, J., Korem, T., Zeevi, D., Zilberman-Schapira, G., Thaiss, C. A., Maza, O., . . . Elinav, E. (2014). Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature, 514(7521), 181-186. doi:10.1038/nature13793
Stevia.com. (2016). How is stevia leaf extract made? Retrieved from: https://www.stevia.com/2016/10/03/how-is-stevia-leaf-extract-made/
Truth in Advertising. (2014). What extra ingredients are in your natural stevia product? Retrieved from: https://www.truthinadvertising.org/extra-ingredients-natural-stevia-product/
U.S. Food & Drug Administration. (2017). Generally recognized as safe (GRAS). Retrieved from: https://www.fda.gov/food/ingredientspackaginglabeling/gras/
Yilmaz, S., & Ucar, A. (2014). A review of the genotoxic and carcinogenic effects of aspartame: does it safe or not? Cytotechnology, 66(6), 875-881. doi:10.1007/s10616-013-9681-0
Wait, I Should Be Eating Bacteria?!
Anessa Helsel, Dietetic Intern 2021

About 45% of American adults suffer from at least one chronic disease (Raghupathi & Raghupathi, 2018). Heart disease, cancer, and diabetes are the leading causes of death in the U.S. (National Center for Chronic Disease Prevention and Health Promotion, 2021). Fortunately, diet plays a huge role in preventing and managing these diseases. It could be as simple as adding fermented foods into your diet. Not only have they been shown to be beneficial in reducing markers of cardiovascular disease, metabolic syndrome, and cancer development, but fermented foods can also improve your health in other ways, too.
What Are Fermented Foods? How Does Bacteria Get in There?
Fermented foods have been around for as long as humans have been eating. Have you ever heard of kefir or kimchi? What about yogurt or beer? These are some examples of foods and drinks that are produced using fermentation. Historically, we have used fermentation as a way to safely preserve food, change the way a food tastes, and even improve digestion. How does this work? When food is stored in conditions that favor the growth of beneficial bacteria, like lactic acid bacteria, these microorganisms “eat” or break down sugar molecules in the food and produce byproducts, some of which can make food safer to consume for longer periods. This process is what spurs the change from cabbage to sauerkraut. When we eat these foods, we also eat the bacteria, and this has been shown to produce beneficial effects in the person eating the food (Marco et al., 2017; Sanlier et al., 2017).
Benefits of Bacteria
Some foods contain compounds that prevent us from absorbing all the vitamins and minerals a food has to offer. Fermentation can help break these types of compounds down so that more nutrients are available for our bodies. But that’s not all fermentation can do! It can also result in the formation of new compounds. Depending on the type of bacteria used during the fermentation process, the resulting product can have increased levels of B vitamins, vitamin C, minerals, like iron, and various amino acids. Consuming these foods with these increased nutrient contents can have awesome effects for us, including decreased inflammation, more neurotransmitter production, support for our immune system, and protection of the GI tract (Marco et al., 2017; Tamang et al., 2016).
Part of the way fermented foods can benefit us is by changing our gut microbiome (Tamang et al., 2016). This has been controversial in the past, but a group of researchers recently looked at almost 7,000 people to see how fermented foods affect the gut microbiome. They looked at stool samples (kind of gross, I know) from all participants and found that people who consumed fermented foods had a more varied gut microbiome than those who didn’t. They also found that people who consumed fermented foods had some of those same microbes in their stool, suggesting that the bacteria from fermented foods colonize the GI tract instead of just passing through (Taylor et al., 2020).
Fermented Milk Could Lower Your Blood Pressure
Many fermented foods have been shown to help with lowering blood pressure, cholesterol, and risk of developing cardiovascular disease. For example, fermented milk products have been shown to lower blood pressure (Marco et al., 2017; Sanlier et al., 2017; Tamang et al., 2016). Drinking milk fermented with a type of lactic acid bacteria just once a day for eight weeks resulted in lowered blood pressure. Researchers even went so far as to say that these fermented milk are as effective as ACE-inhibitors, which are medications prescribed to reduce blood pressure (Beltran-Barrientos et al., 2016)! Another study looked at the same type of fermented milk and found that drinking just over a half cup a day lowered blood pressure in participants diagnosed with high blood pressure after 21 weeks (Seppo et al., 2003). Parts of milk proteins can lower blood pressure, but they have to be “activated” and released from the rest of the protein to do so. If our bodies are unable to do that, the bacteria in fermented milks can. Plus, the fermentation process increases the milk’s calcium and potassium content, which is also helpful in lowering blood pressure (Beltran-Barrientos et al., 2016; Seppo et al., 2003).
Fermented Veggies – Tasty and Good For You
Fermented foods can help lower cholesterol, too. Kimchi is a staple of the Korean diet. It is a fermented vegetable side dish made with cabbage, radishes, spices, and fish sauce (Sanlier et al., 2017). It is already well known that kimchi can reduce plaque formation in your arteries, oxidation, and inflammation, all of which can contribute to cardiovascular disease. But it can also reduce high cholesterol. After eating 210 grams of kimchi a day for seven days, study participants had lowered their total cholesterol levels significantly more than those eating only 15 grams of kimchi per day. The only thing different about the two groups was how much kimchi they ate; otherwise, they ate the same meals and maintained their normal levels of physical activity (or inactivity). Researchers also found improvements in markers of diabetes in the group eating more kimchi (Choi et al., 2013). Changing just one thing you eat can make a significant improvement to your health.
Fermented Foods Can Help Your Heart
The types of bacteria you have in your gut may influence how healthy, or diseased, you are. Your gut microbiota sends signals to the rest of your body, and researchers have found that people with cardiovascular disease may have types of gut bacteria that send signals to promote inflammation, which is linked with many types of chronic disease, only one of them being heart disease. These signals may even play a role in contributing to high blood pressure (Tang et al., 2017).
High blood pressure and high cholesterol are both risk factors for cardiovascular disease. Men and women with hypertension who ate at least two servings of yogurt per week were found to have a lower risk of developing cardiovascular disease. However, the lowest risk was seen in those who were also eating a balanced diet full of fruits, vegetables, lean protein, and an abundance of vitamins and minerals (Buendia et al., 2018). While fermented foods have great benefits, they’re not a cure-all; they should be part of a balanced diet for you to get the most benefit from them.
Diabetes and Diet – Are Fermented Foods an Answer?
We all know someone who has been diagnosed with type 2 diabetes, but what causes it? Negative changes in the type of bacteria in your gut could be a part of the problem. Researchers have found that people with type 2 diabetes have a smaller amount of the good bacteria and a larger amount of bad bacteria in their guts than people without diabetes. This can lead to significant changes in how our body functions (Wang et al., 2020).
If a “bad” gut microbiota can potentially cause diabetes, can a “good” gut microbiota help fix diabetes? Let’s look at the research. Kefir (fermented milk), kimchi, and other fermented foods have been shown to have some anti-diabetic properties (Marco et al., 2017; Sanlier et al., 2017). Some of these foods can help your body be more responsive to insulin, the hormone that lets glucose enter your cells (Tamang et al., 2016). It looks like consuming fresh kimchi (essentially vegetables) for eight weeks can help lower your weight and waist circumference. That’s pretty cool! But what’s really cool is that consuming fermented kimchi can decrease insulin resistance and increase insulin sensitivity, hopefully making diabetes easier to manage (An et al., 2013). Another study found that when people with type 2 diabetes drank 20 ounces (the size of a bottle of soda) of kefir for eight weeks, their bodies produced more insulin and were more responsive to it, which led to lower hemoglobin A1C values and better control of diabetes (Sivamaruthi et al., 2018).
Fermented Foods versus Cancer
Cancer is a big, scary disease. It seems like there is so much conflicting information out there on how to prevent cancer and how to treat it if you have it. Luckily, it seems like some foods fermented with lactic acid bacteria have anti-cancer properties and may be able to slow the spread of some cancers (Tamang et al., 2016). These beneficial bacteria can change your gut microbiome, helping to strengthen your immune system and prevent cancer from starting in the first place. Kimchi, which is often fermented with lactic acid bacteria, has been found to turn off proteins that help activate cancerous cells. The good bacteria we eat with kimchi survive your digestion and can stop the bad bacteria from sticking to your intestinal cells, preventing them from becoming cancerous in the first place (Kwak et al., 2014).
Now What?
Fermented foods have many beneficial properties and have been shown to have positive effects on many chronic diseases. They also have been shown to improve gut health, which we are learning also affects the development of chronic disease. Try adding fermented foods into your diet today – or experiment with making them at home!
References
An, S., Lee, M. S., Jeon, J. Y., Ha, E. S., Kim, T. H., Yoon, J. Y., Ok, C., Lee, H., Hwang, W., Choe, S. J., Han, S. J., Kim, H. J., Kim, D. J., & Lee, K. (2013). Beneficial effects of fresh and fermented kimchi in prediabetic individuals. Annals of Nutrition and Metabolism, 63, 111-119. https://doi.org/10.1159/000353583
Beltran-Barrientos, L. M., Hernandez-Mendoza, A., Torres-Llanez, M. J., Gonzalez-Cordova, A. F., & Vallejo-Cordoba, B. (2016). Invited review: Fermented milk as an antihypertensive functional food. Journal of Diary Science, 99(6), 4099-4110. https://doi.org/10.3168/jds.2015-10054
Buendia, J. R., Li, Y., Hu, F. B., Cabral, H. J., Bradlee, M. L., Quatromoni, P. A., Singer, M. R., Curhan, G. C., & Moore, L. L. (2018). Regular yogurt intake and risk of cardiovascular disease among hypertensive adults. American Journal of Hypertension, 31(5), 557-565. https://doi.org/10.1093/ajh/hpx220
Choi, I. H., Noh, J. S., Han, J., Kim, H. J., Han, E., & Song, Y. O. (2013). Kimchi, a fermented vegetable, improves serum lipid profiles in healthy young adults: Randomized clinical trial. Journal of Medicinal Food, 16(3), 223-229. https://doi.org/10.1089/jmf.2012.2563
Kwak, S., Cho, Y., Noh, G., & Om, A. (2014). Cancer preventive potential of kimchi lactic acid bacteria (Weissella cibaria, Lactobacillus plantarum). Journal of Cancer Prevention, 19(4), 253-258. https://doi.org/10.15430/JCP.2014.19.4.253
Marco, M. L., Heeney, D., Binda, S., Cifelli, C. J., Cotter, P. D., Foligne, B., Ganzale, M., Kort, R., Pasin, G., Pihlanto, A., Smid, E. J., & Hutkins, R. (2017). Health benefits of fermented foods: Microbiota and beyond. Current Opinion in Biotechnology, 44, 94-102. https://doi.org/10.1016/j.copbio.2016.11.010
National Center for Chronic Disease Prevention and Health Promotion. (2021, April 28). About chronic diseases. Centers for disease control and prevention. https://www.cdc.gov/chronicdisease/about/index.htm#:~:text=Chronic%20di….
Raghupathi, W., & Raghupathi, V. (2018). An empirical study of chronic diseases in the United States: A visual analytics approach to public health. International Journal of Environmental Research and Public Health, 15(3), 431. https://doi.org/10.3390/ijerph15030431
Sanlier, N., Gokcen, B. B., & Sezgin, A. C. (2017). Health benefits of fermented foods. Critical Reviews in Food Science and Nutrition, 59(3), 506-527. https://doi.org/10.1080/10408398.2017.1383355
Seppo, L., Juahiainen, T., Poussa, T., & Korpela, R. (2003). A fermented milk high in bioactive peptides has a blood pressure-lowering effect in hypertensive subjects. The American Journal of Clinical Nutrition, 77(2), 326-330. https://doi.org/10.1093/ajcn/77.2.326
Sivamaruthi, B. S., Kesika, P., Prasanth, M. I., & Chaiyasut, C. (2018). A mini review on the antidiabetic properties of fermented foods. Nutrients, 10(12), 1973. https://doi.org/10.3390/nu10121973
Tamang, J. P., Shin, D., Jun, S., & Chae, S. (2016). Functional properties of microorganisms in fermented foods. Frontiers in Microbiology, 7(58). https://doi.org/10.3389/fmicb.2016.00578
Tang, W. H. W., Kitai, T., & Hazen, S. L. (2017). Gut microbiota in cardiovascular health and disease. Circulation Research, 120(7), 1183-1196. https://doi.org/10.1161/CIRCRESAHA.117.309715
Taylor, B. C., Lejzerowicz, F., Poirel, M., Shaffer, J. P., Jiang, L., Aksenov, A., Litwin, N., Humphrey, G., Martino, C., Miller-Montgomery, S., Dorrestein, P. C., Veiga, P., Song, S. J., McDonald, D., Derrien, M., & Knight, R. (2020). Consumption of fermented foods is associated with systematic differences in the gut microbiome and metabolome. mSystems, 5(2), e00901-19. https://doi.org/10.1128/mSystems.00901-19
Wang, P., Deng, X., Zhang, C., & Yuan, H. (2020). Gut microbiota and metabolic syndrome. Chinese Medical Journal, 133(7), 808-816. https://doi.org/10.1097/CM9.0000000000000696
The Nutritional Benefits of Sourdough Bread
Audrey Bogue, Dietetic Intern 2017

Traditional sourdough breads are made with lactic acid bacteria and naturally occurring yeasts. These ingredients are then fermented; a long, slow ferment is recommended for the most health benefits. This process does produce probiotics, however, these probiotics are destroyed during the baking process. But the good news is that recent studies show that killed probiotics may have positive effects on health! Even though sourdough doesn't contain probiotics, it does contain exopolysaccharides, which acts as a prebiotic to feed the good intestinal bacteria (Poutanen, Flander, & Katina, 2009). The breads that have a longer ferment have no need for additional leavening agents, including baking soda or brewers yeast. These breads can be made with only 4 simple ingredients: flour, water, salt, and a sourdough starter. If you are making sourdough at home, a sourdough starter can be made or purchased (Marco et al., 2017).
Improved Digestibility
The long, slow fermentation process helps break down carbohydrates. It decreases the fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FOD-MAPS) that are found in breads. The reduced FOD-MAP content in sourdough bread improves the digestibility of the bread. This means that patients with IBS may be able to tolerate sourdough breads! Food trials are necessary to determine if a patient with IBS can tolerate sourdough (Poutanen, Flander, & Katina, 2009).
Sourdough breads have also been shown to have a reduced gluten content. The decreased pH during fermentation causes gluten degradation. The reduced gluten content of sourdough may improve digestion too! It is important to note that individuals with celiac disease, non-celiac wheat sensitivity, and other forms of gluten intolerance still cannot properly digest the gluten found in sourdough breads (Poutanen, Flander, & Katina, 2009). However, sourdough breads can be made from gluten-free flours! The sourdough fermentation of gluten-free products improves the taste, texture, and can even delay the onset of staling. So you can still receive the health benefits of sourdough even on a gluten-free diet (Rizzello, Lorusso, Montemurro, &Gobbetti, 2016).
Phytic Acid
Phytic acid (PA)is a chemical compound that act as anti-nutrients in the body because it inhibits the absorption of certain minerals including calcium, magnesium, zinc, and iron (Lopez et al., 2003).The PA binds to these minerals forming phytates, which cannot be absorbed by the body. These phytates pass through the intestinal track unabsorbed and these important minerals are excreted. PA is found in high amounts in many whole-grain products including traditional breads. Even when sourdough bread is made from the same flour as conventional bread, it has a lower PA content. This is due to the lactic acid bacteria lowering the pH of the bread, which causes phytate hydrolysis that reduces the PA content of the bread (Leenhardt, Levrat-Verny, Chanliaud, &Rémésy, 2005).This means that the minerals found in sourdough bread can be absorbed and utilized in the body!
Glycemic Index
The glycemic index is a measure of the rise in blood glucose after a food is consumed. Foods that are high in carbohydrates and low infiber typically have a high glycemic index. Traditional white bread has a glycemic index of 70. Studies show that sourdough breads made from both white flour and whole-wheat flour have a lower glycemic index than the traditional counterparts. Individuals with type 1 and type 2 diabetes mellitus, should be aware of food with a high glycemic index because it can cause a rapid rise in blood glucose(De Angelis et al., 2007). In a recent study of healthy participants, sourdough's effects on postprandial glycemic and insulin responses were evaluated. This study compared sourdough bread leavened with lactobacilli and a normal bread leavened with baker's yeast. This study found that the participants who received the sourdough bread had lower plasma glucose and lower plasma insulin responses (Maioli et al., 2008). This means that patients with impaired glucose metabolism, like diabetes, may benefit from consuming sourdough bread!
Overall, sourdough breads can be a great addition to a healthy and balanced diet. Sourdough breads unique fermentation helps improve mineral bioavailability and digestibly, while lowering the phytic acid content and the glycemic index. So whether you enjoy sourdough breads for their health benefits or for it's delicious flavor, choosing to go sour can actually be a pretty sweet deal!
References
Bartkiene, E., Juodeikiene, G., Vidmantiene, D., Viskelis, P., &Urbonaviciene, D. (2011). Nutritional and quality aspects of wheat sourdough bread using L. luteus and L. angustifolius flours fermented by Pedioccocusacidilactici. International Journal of Food Science and Technology, 46(8), 1724-1733.
Bryszewska, M. A., Ambroziak, W., Diowksz, A., Baxter, M. J., Langford, N. J., & Lewis, D. J. (2005). Changes in the chemical form of selenium observed during the manufacture of a selenium-enriched sourdough bread for use in a human nutrition study. Food Additives and Contaminants, 22(2), 135-140.
De Angelis, M., Rizzello, C. G., Alfonsi, G., Arnault, P., Cappelle, S., Di Cagno, R., &Gobbetti, M. (2007).Use of sourdough lactobacilli and oat fibre to decrease the glycaemic index of white wheat bread.British Journal of Nutrition, 98(06), 1196-1205.
Leenhardt, F., Levrat-Verny, M. A., Chanliaud, E., &Rémésy, C. (2005). Moderate decrease of pH by sourdough fermentation is sufficient to reduce phytate content of whole wheat flour through endogenous phytase activity. Journal of Agricultural and Food Chemistry, 53(1), 98-102.
Lopez, H. W., Duclos, V., Coudray, C., Krespine, V., Feillet-Coudray, C., Messager, A., &Rémésy, C. (2003). Making bread with sourdough improves mineral bioavailability from reconstituted whole wheat flour in rats. Nutrition, 19(6), 524-530.
Maioli, M., Pes, G. M., Sanna, M., Cherchi, S., Dettori, M., Manca, E., & Farris, G. A. (2008). Sourdough-leavened bread improves postprandial glucose and insulin plasma levels in subjects with impaired glucose tolerance. ActaDiabetologica, 45(2), 91-96.
Marco, M. L., Heeney, D., Binda, S., Cifelli, C. J., Cotter, P. D., Foligné, B., &Smid, E. J. (2017). Health benefits of fermented foods: Microbiota and beyond. Current Opinion in Biotechnology, 44(1), 94-102.
Poutanen, K., Flander, L., & Katina, K. (2009). Sourdough and cereal fermentation in a nutritional perspective.Food Microbiology, 26(7), 693-699.
Rizzello, C. G., Lorusso, A., Montemurro, M., &Gobbetti, M. (2016). Use of sourdough made with quinoa (Chenopodium quinoa) flour and autochthonous selected lactic acid bacteria for enhancing the nutritional, textural and sensory features of white bread. Food Microbiology, 56(1), 1-13.
Scazzina, F., Del Rio, D., Pellegrini, N., &Brighenti, F. (2009). Sourdough bread: Starch digestibility and postprandial glycemic response. Journal of Cereal Science, 49(3), 419-421.
Tucker, A. J., MacKay, K. A., Robinson, L. E., Graham, T. E., Bakovic, M., & Duncan, A. M. (2010). The effect of whole grain wheat sourdough bread consumption on serum lipids in healthy normoglycemic/normoinsulinemic and hyperglycemic/hyperinsulinemic adults depends on presence of the APOE E3/E3 genotype: A randomized controlled trial. Nutrition and Metabolism, 7(1), 37-50.
Hypothyroidism and the Detrimental Duo
Katrina Thomas, Dietetic Intern 2022

If you're reading this, then it's likely that your child is suffering from hypothyroidism, and you want to help. You're in luck! I will be informing you of two food items that could positively change your child's experience with hypothyroidism. But, first, I'd like to tell you a little about myself and why I'm so passionate about helping you help your child overcome certain hurdles hypothyroidism might produce.
It’s Not Sympathy, Its Empathy: Here’s My Story
Since I was eight years old, I began gaining weight each year, not just a little weight, 30 to 40 pounds per year. That's when it happened; for lack of a better term, I became the fat kid everyone made fun of. My mother was frantic because doctors could not explain why I was gaining so much weight since I didn't eat an overabundance of food.
Fast forward to adulthood; I was around 22 years old when I discovered that hypothyroidism was one of the primary players in my life story. I struggled with so many symptoms, which included:
- Weight gain
- Fatigue
- Irritability
- Depression
- Hair loss
- Cold sensitivity
- Muscle weakness
- Trouble concentrating and more.
All my symptoms contributed to what seemed like a lifetime of feeling like an outsider. Yet somehow, it felt better to finally be able to put a name to the condition that had caused me so much pain.
You Have More Control Than You Think
I say all that to say I know first-hand how it feels to struggle with hypothyroidism. I’m sure there are days that you feel helpless as a parent to a child with this condition, but we can get through this monumental time in your child’s life together.
The truth is you're not helpless, and there are foods you can eliminate from your child's diet that can alter their experience with hypothyroidism. In addition, since your child has been diagnosed with hypothyroidism, it's likely that they also suffer from Hashimoto’s disease.
Hashimoto's is an autoimmune disease that causes the thyroid gland to attack its healthy thyroid hormone-producing cells (Chiovato et al., 2019). The destruction of the thyroid gland caused by the autoimmune disease causes hypothyroidism in most cases. Gluten and dairy are two detrimental foods that negatively affect your child’s condition and their overall thyroid health. Ask your child's doctor to check thyroid peroxidase antibodies to determine if their hypothyroidism is caused by Hashimoto's.
Let’s Talk about Gluten!
Gluten refers to the proteins found in wheat, rye, barley, and triticale - a cross between wheat and rye. By acting as a glue, gluten helps food maintain its shape. As a result, many foods contain gluten, including those you would not expect. Gluten is primarily found in:
- bread
- baked goods
- soups
- pasta
- cereals
- sauces
- salad dressings
- roux (CDF, n.d.)
Gluten Could Be Affecting Your Child’s Thyroid Health

Gluten intake is detrimental for individuals who are genetically prone to autoimmune conditions, such as Hashimoto’s disease. Once gluten is detected in the gut, your body produces enzymes to help digest it, signaling their immune cells to cause inflammation (GiG, 2019). Autoimmune conditions are chronic, but thankfully their symptoms and severity can be reduced through diet and lifestyle changes, such as the moderation or elimination of highly inflammatory foods.
Celiac disease is an autoimmune disorder that damages the small intestine, triggered by gluten-containing foods (Murray, n.d.). People with one autoimmune disorder often suffer from multiple autoimmune conditions, so it is essential to rule out Celiac disease before indicating the impact that gluten has on patients with Hashimoto’s.
In addition, there is another common condition associated with gluten intake called non-celiac gluten sensitivity (NCGS), which is often self-diagnosed, making it difficult to establish its true prevalence (Rashid, 2021). Although people with NCGS could have one or more symptoms, including bloating, abdominal pain, and diarrhea, symptoms like irritable bowel syndrome sometimes occur. Aside from nausea and constipation, other intestinal symptoms include acid reflux, mouth ulcers, and acid reflux. Other symptoms may include fatigue, headaches, foggy thinking, numbness, joint pains, skin rashes, and intestinal symptoms.
There are Studies to Suggest It
In one study, a group of researchers tested if a gluten-free diet could positively affect the thyroid's activity, function, and autoimmunity (Krysiak et al., 2019). Thirty-four women with Hashimoto's disease were divided into two groups. Sixteen women followed a gluten-free diet for six months, while the remaining women ate their regular diets. The women provided blood samples to investigate their thyroglobulin antibodies, thyroid peroxidase, thyrotropin, vitamin D, and free thyroid hormone levels. The study's results indicated that all the levels stayed within similar ranges except for reductions in thyroglobulin antibodies and increased vitamin D levels in the women who followed the gluten-free diet. In addition, the study's researchers determined that the gluten-free diet successfully reduced the autoimmunity of the thyroid and increased its output.
Not Convinced? Here’s One More
In another study, a research team tested if a gluten-free diet would be effective in individuals with Hashimoto’s disease (Pobłocki et al., 2021). Sixty-two women were equally divided into two groups. Half of them followed a twelve-month-long gluten-free diet, while the other half received no intervention. All the participants supplied blood samples to determine their thyroid hormone concentrations and antibodies at baseline and then at their three, six, and twelve-month check-ups. The results indicated that the group that adhered to the gluten-free diet experienced significant reductions in their TSH levels while increasing their free thyroxine hormones. Although the study concluded that further research needed to be conducted, the participants who adhered to the gluten-free diet experienced some improvement in their thyroid function.
Ditching the Dairy Could Help Make Your Child’s Condition Less Scary?
As far as dairy is concerned, there are two milk-related conditions to be aware of as a parent of a child with Hashimoto's.
Dairy or cow's milk allergy is among the most common food allergies (DerSarkissian, 2021). As a result, anaphylaxis due to milk allergy is among the most common worldwide. This condition is caused by an immune system reaction triggered by proteins in cow's milk. As part of the body's defense system, when the immune system detects a specific protein in milk, it sends an immune response to destroy the threat. However, if the immune system encounters the same protein in the future, it releases chemicals that trigger cow's milk allergy symptoms. This disease mainly affects children in their first year of life and usually regresses by age six. The condition is commonly treated with a dairy-free diet.
The second condition is lactose intolerance, which is caused by insufficient lactase enzyme in a person's small intestine, which is necessary to digest milk sugar (lactose) (Mayo Clinic, 2022). Under normal conditions, digested lactose turns milk sugar into simple sugars known as glucose and galactose. The intestinal lining absorbs simple sugars into the bloodstream. Yet, if a person has a lactase deficiency, unabsorbed/unprocessed lactose moves into the colon instead. Therefore, normal bacteria interact with undigested lactose, causing lactose intolerance.
Proteins found in animal milk are like human proteins due to their compositions, which might explain why milk triggers inflammation in some humans. Most digestive problems are caused by certain proteins found in dairy. Intolerance to milk products will result in the immune system recognizing milk proteins and reacting to them. Even when no animal milk is being digested, immune cells sometimes look for similar proteins. It is possible to find similar proteins in thyroid cells, which causes an autoimmune response.
The autoimmune thyroid problem is not caused by lactose but may cause issues for lactose intolerant people (Endocrine Society, 2019). Some thyroid medications contain lactose, which could be especially problematic for people with a more severe form of lactose intolerance.
How Dairy Affected the Participants in This Study

In this study, researchers measured the prevalence of lactose intolerance in patients with Hashimoto's and how lactose restriction impacted their thyroid function (Asik et al., 2014). Fifty patients with Hashimoto's who took L-thyroxine medication were used to determine the effectiveness of the study. Thirty-eight patients were lactose intolerant and on a lactose-restricted diet for eight weeks. Thirty had normal thyroid function, while eight had subclinical hypothyroidism, meaning they had mildly elevated TSH levels. On the other hand, the remaining twelve did not have lactose intolerance, yet they were placed on the same diet. The study's results indicated that the thirty-eight lactose-intolerant participants experienced significantly lower TSH levels. Contrarily, the twelve participants who did not have lactose intolerance had little change in their TSH levels. The team determined that low levels of TSH are associated with lactose restriction. Therefore, hypothyroid patients with irregular TSH levels, increased LT4 doses, or inadequate response to LT4 treatment should consider lactose intolerance as the culprit.
Why Risk it When You Can Ditch It?
Gluten and dairy are not enemies, but they represent a duo that can be detrimental to your child’s thyroid health. So, the true question is, why risk your child’s thyroid function to the harmful inflammatory effects of gluten and dairy?
You can ditch them both and enjoy the road to better thyroid health for your child and peace of mind for you.
Ditching the duo is a journey, not a marathon, so health professionals are there to help you and your child along the way. For example, if you decide you'd like to check if going gluten-free would help your child attain better thyroid function, there are professionals available to help you. Let one of your child’s healthcare professionals know your concerns so they can give you the proper referral.
What You Should Expect When Getting Help
Firstly, a professional would work with you to place them on a gluten-rich diet for around six weeks while under the supervision of a healthcare professional who performs blood and skin tests to rule out celiac disease. Secondly, they would inform you to exclude gluten from their diet for around six weeks while keeping a detailed record of all their symptoms, including those that are secondary to their Hashimoto's disease. Thirdly, if their previous symptoms and lab work showed improvement, they would gradually reintroduce gluten and/or dairy-containing food (one at a time) into the diet. Yet, if their symptoms reemerge or the thyroid function decreases, they will let you know if your child should remain gluten and/or dairy-free. The gluten-free and/or dairy-free diets may not be meant for all people with Hashimoto’s, yet if you're willing to help your child comply with the diet, it is worth a try.
The appointments will let you know if your child has Celiac disease or non-celiac gluten sensitivity and how gluten affects your child’s thyroid health. After the appointments, you can decide whether you want to keep them on a gluten-free diet permanently or for a trial period.
References
Asik, M., Gunes, F., Binnetoglu, E., Eroglu, M., Bozkurt, N., Sen, H., Akbal, E., Bakar, C., Beyazit, Y., & Ukinc, K. (2014). Decrease in TSH levels after lactose restriction in Hashimoto's thyroiditis patients with lactose intolerance. Endocrine, 46(2), 279–284. https://doi.org/10.1007/s12020-013-0065-1
CDF. (n.d.). What is gluten? Celiac Disease Foundation. Retrieved June 21, 2022, from https://celiac.org/gluten-free-living/what-is-gluten/#:~:text=Gluten%20….
Chiovato, L., Magri, F., & Carlé, A. (2019). Hypothyroidism in context: Where we've
been and where we're going. Advances in Therapy, 36(Suppl 2), 47–58. https://doi.org/10.1007/s12325-019-01080-8
DerSarkissian, C. (2021, June 9). Lactose intolerance vs. dairy allergy: Symptoms,
diagnosis, living with. WebMD. Retrieved July 7, 2022, from https://www.webmd.com/digestive-disorders/lactose-intolerance-or-dairy-…
Endocrine Society. (2019, November 15). Cow's milk interferes with absorption of thyroid supplement levothyroxine. Endocrine Society. Retrieved June 21, 2022, from https://www.endocrine.org/news-and-advocacy/news-room/2017/cows-milk-in…
GiG. (2019, October 17). Celiac disease & thyroid conditions. Gluten Intolerance group. Retrieved June 21, 2022, from https://gluten.org/2019/10/17/celiac-disease-thyroid-conditions/
Krysiak, R., Szkróbka, W., & Okopień, B. (2019). The effect of gluten-free diet on
thyroid autoimmunity in drug-naïve women with Hashimoto’s thyroiditis: A Pilot Study. Experimental and clinical endocrinology & diabetes: official journal, German Society of Endocrinology [and] German Diabetes Association, 127(7), 417–422. https://doi.org/10.1055/a-0653-7108
Mayo Clinic. (2022, March 5). Lactose intolerance. Mayo Clinic. Retrieved June 21, 2022, from https://www.mayoclinic.org/diseases-conditions/lactose-intolerance/symp…
Murray, J. A. (n.d.). Celiac disease. National Institute of diabetes and digestive and kidney diseases. Retrieved June 21, 2022, from https://www.niddk.nih.gov/health-information/digestive-diseases/celiac-….
Pobłocki, J., Pańka, T., Szczuko, M., Telesiński, A., & Syrenicz, A. (2021). Whether a
gluten-free diet should be recommended in chronic autoimmune thyroiditis or not? -a 12-month follow-up. Journal of Clinical Medicine, 10(15), 3240. https://doi.org/10.3390/jcm10153240
Rashid, M. (2021, December 13). Non-celiac gluten sensitivity. Canadian Celiac Association. Retrieved July 7, 2022, from https://www.celiac.ca/gluten-related-disorders/non-celiac-gluten-sensit…
A Non-Diet Approach to Weight Loss and Dieting Myths Debunked
Nathan Slinkard, Dietetic Intern 2018

The ever-elusive goal of sustained weight loss has been chased by so many Americans with varying degrees of success and failure (at least 80% fail). Weight loss frenzy has caused food producers, doctors, and "health" companies to create pills and concoctions and plans to help us tighten our belts. But why are so many Americans still obese? Why do dieters fail so often? Hasn't someone figured out the perfect weight loss diet by now? Although the weight loss industry in America has suffered some losses in recent years due to disdain for diet products and weight-loss programs, it still amassed $64 billion in revenue in 2014.1 Other weight loss avenues such as bariatric surgery and health club memberships have risen in popularity. In this blog, we'll take a look at some of the reasons why weight loss can be so challenging and some strategies that work for the majority of people. But here's a spoiler alert: everyone is different and no one approach fits all.
The Myth That Cutting 3500 Calories a Week Results in One Pound of Fat Loss
A widespread generalization still popular today, is that one pound of body fat is equivalent to 3500 calories. The reason why this is an inaccurate assumption is that everyone is different and, thermodynamically speaking, the body digests and stores food at a rate unique to the individual. Furthermore, the trillions of bacteria in our guts can even impact how many calories we absorb. A review of seven closely-controlled clinical weight loss studies tested the accuracy of the 3500 calorie rule.2 The participants, who were monitored at all times, restricted calories over an average of 64.8 days with an average deficit of 1,409 calories. If 3500 calories mean one pound of weight loss, the participants should have lost an average of 27.6 pounds. However, they lost an average of 20.1 pounds plus or minus a huge range of 12.6 pounds. This brings up an important point which we'll discuss next: why do dieters hit plateaus during their weight loss journeys?
Cutting Calories and Adaptive Thermogenesis
This point frustrates many to no end and leads to feelings of hopelessness. I'm referring to the "wall" that calorie cutters often hit after just one or two weeks of quick weight loss. This can be attributed to how our body's metabolism slows in response to weight loss. Research has shown that energy expenditure slows by 20-25% after a 10% reduction in body weight, mostly due to a change in non-resting energy expenditure. That's an extra 10-15% fewer calories than we expend beyond what might have been predicted by recalculating energy expenditure.3 This is due to a complex, coordinated reaction by our bodies that involves many neuroendocrine and metabolic pathways.
Thrifty Genes and the Set Point Theory
The Thrifty Gene Hypothesis claims that this modern weight loss conundrum can be explained by "thrifty genes" that efficiently store food as fat in times of reduced calorie consumption. Our ancestors lacked the luxury of grocery stores and fast-food restaurants and had frequent food shortages. The idea then is that our bodies have evolved to efficiently store food as body fat in times of famine. A society in which we no longer forage or hunt for food has fueled an overabundance of this storage! Another well-known ideology, the Set Point Theory, says that each individual has a fairly narrow range of weight that their body is comfortable with. Any weight change, whether gained or lost, will result in the body fighting against this with shifts in metabolism. Perhaps those that tend to carry a little extra weight were never really meant to lose it. So, how is it possible to lose weight and keep it off when our bodies seem to be fighting against us? The resounding answer is that sustained weight loss must involve lifestyle changes.
Why Lifestyle Changes Are More Important Than a Diet
A large study conducted in Australia sought to determine how effective or detrimental habitual dieting is for weight loss. They adjusted the data for initial BMI (Body Mass Index) and tracked what happened over the following 12 months.4 Amazingly, the risk of developing obesity was 1.9, 2.9, or 3.2 times higher for those that dieted once, more than once, and always, respectively, versus non-dieters. Non-dieters had much better odds of maintaining their BMI or reducing it compared to dieters. Whoa! The researchers copied what many health professionals preach by saying that "losing weight requires a commitment to change one's lifestyle and a sustained effort to maintain a healthy diet and engage in physical activity". That's right, folks! It is nearly impossible to keep weight off without making some lasting changes. This is not to say that every diet approach is ineffective, and it is important to determine which pattern of eating is most effective for you.
No Diet Works for Everyone
If habitual dieting has a poor track record, what has been effective? One of the hottest trends is the ketogenic diet which keeps your fats very high (around 80% of your calories), your protein pretty moderate (~10-20%), and your carbs extremely low (~20-50 grams per day). The ketogenic diet has shown to be very effective for some.5 However, low-fat vegan and vegetarian diets, at the opposite end of the scale, have also been shown to promote great weight loss results.6 So, wait, which diet, as you're asking right now, is better? Even more important questions to ask, though, are "why did these diets fail some participants?" and "would you fall into this group?" The answer to the first question, as you probably guessed, is that everyone is different. There is exciting new research on how personalizing diet based on an individual's genetics, also known as nutrigenomics, can help reduce the risk of developing conditions like obesity.7, 8, 9, 10 However, personalized nutrition based on genetics has certainly experienced some growing pains. The second question, then, is harder to answer and may very well take some trial-and-error. By no means, though, should you have to do this all on your own. Nutrition counseling is ideal, especially when navigating the field of nutrigenomics, and is helpful for weight loss in both group and individual formats.11
Lifestyle Changes to Implement and a Brief Conclusion
The most effective weight loss strategies center around improving sleep, reducing stress, getting off the couch and moving around more, and eating a diet low in processed foods and loaded with vegetables. Often the reason why studies show great results for vastly different diets (such as the Mediterranean or the vegan or the ketogenic) is that participants go from eating a standard American junk food diet to making conscious decisions about what they put into their bodies. If you go from eating McDonald's to tofu or salmon or a grass-fed avocado burger, then you have a pretty decent chance of losing belly fat! These diets often have overlapping core principles like choosing whole foods, real foods, and food products with fewer ingredients. These, along with the following tips, are time-honored approaches to better health. Increase your physical activity to boost your metabolism and practice mindful eating to help avoid overeating. Drink plenty of water for its health benefits like helping to prevent headaches and constipation, but also for its potential impact on weight loss itself and because thirst may be misinterpreted by the body as hunger.12, 13 Keep track of how your diet is impacting your lab values, and investigate the underlying problem if you fail to lose weight such as sleep apnea and hormonal imbalances. Rely on friends and family for support and seek nutritional counseling for guidance, especially with regards to optimizing diet based on genetic testing.
In conclusion, remember to not expect exactly one pound of weight loss for every 3500 calories that you cut. Know that the human body adapts to weight loss by adjusting metabolic rates and that it may be an uphill battle because of our evolution and genetics. But take heart, because you know a secret that failing dieters are not accepting: smart, lifestyle changes triumph over habitual on and off dieting for sustained weight loss results.
References
1. Kell J. Lean times for the diet industry. Fortune. http://fortune.com/2015/05/22/lean-times-for-the-diet-industry/. Published May 22, 2015.
2. Thomas DM, Martin CK, Lettieri S, et al. Can a weight loss of one pound a week be achieved with a 3500-kcal deficit? Commentary on a commonly accepted rule. International Journal of Obesity. 2013;37(12):1611-1613. doi:10.1038/ijo.2013.51.
3. Rosenbaum M, Leibel RL. Adaptive thermogenesis in humans. International journal of obesity (2005). 2010;34(0 1):S47-S55. doi:10.1038/ijo.2010.184.
4. Siahpush M, Tibbits M, Shaikh R, Singh G, Sikora Kessler A, Huang T. Dieting Increases the Likelihood of Subsequent Obesity and BMI Gain: Results from a Prospective Study of an Australian National Sample. International Journal Of Behavioral Medicine [serial online]. October 2015;22(5):662-671. Available from: SPORTDiscus with Full Text, Ipswich, MA. Accessed April 14, 2018.
5. Dashti HM, Mathew TC, Hussein T, et al. Long-term effects of a ketogenic diet in obese patients. Experimental & Clinical Cardiology. 2004;9(3):200-205.
6. Huang R, Huang C, Hu F, Chavarro J. Vegetarian Diets and Weight Reduction: a Meta-Analysis of Randomized Controlled Trials. Journal Of General Internal Medicine [serial online]. January 2016;31(1):109-116. Available from: MEDLINE, Ipswich, MA. Accessed April 15, 2018
7. Luan J, Browne P, Wareham N, et al. Evidence for Gene-Nutrient Interaction at the PPAR lambda Locus. Diabetes [serial online]. March 2001;50(3):686. Available from: Academic Search Complete, Ipswich, MA. Accessed April 15, 2018.
8. Moleres A, Ochoa M, Marti A, et al. Dietary fatty acid distribution modifies obesity risk linked to the rs9939609 polymorphism of the fat mass and obesity-associated gene in a Spanish case-control study of children. The British Journal Of Nutrition [serial online]. February 2012;107(4):533-538. Available from: MEDLINE, Ipswich, MA. Accessed April 15, 2018.
9. Kourlaba G, Kondaki K, Grammatikaki E, et al. Interaction effects between total energy and macronutrient intakes and angiotensin-converting enzyme 1 (ACE) I/D polymorphism on adiposity-related phenotypes in toddlers and preschoolers: the Growth, Exercise and Nutrition Epidemiological Study in preSchoolers (GENESIS). British Journal Of Nutrition [serial online]. December 2008;100(6):1333-1340. Available from: Agricola, Ipswich, MA. Accessed April 15, 2018.
10. Qi Q, Sacks F, Qi L, Bray G, Hu F. Weight-loss diets modify glucose-dependent insulinotropic polypeptide receptor rs2287019 genotype effects on changes in body weight, fasting glucose, and insulin resistance: the Preventing Overweight Using Novel Dietary Strategies trial. American Journal Of Clinical Nutrition [serial online]. February 2012;95(2):506-513. Available from: Agricola, Ipswich, MA. Accessed April 15, 2018.
11. Phimarn W, Paktipat P, Pansiri K, Klabklang P, Duangjanchot P, Tongkul A. Effect of Weight Control Counselling in Overweight and Obese Young Adults. Indian Journal Of Pharmaceutical Sciences [serial online]. January 2017;79(1):35-41. Available from: Academic Search Complete, Ipswich, MA. Accessed April 14, 2018.
12. Chang T, Ravi N, Plegue MA, Sonneville KR, Davis MM. Inadequate Hydration, BMI, and Obesity Among US Adults: NHANES 2009-2012. Ann Fam Med. 2016:320-324. doi:10.1370/afm.1951. Introduction.
13. Marshall M. The big benefits of plain water. Harvard Health Blog. https://www.health.harvard.edu/blog/big-benefits-plain-water-201605269675. Published May 13, 2016. Accessed April 15, 2018.
Say Good-Bye to Eating Rules
Tiffany Kroll, Dietetic Intern 2017
Intuitive Eating is the non-diet approach to help individuals relearn how to eat in response to internal, rather than external cues (Bush et al, 2014). It is learning to listen to your body, rather than ignoring those inner cues - you know, that tell you when you are hungry and when you are full. It isn't restrictive eating, it is relying on your body to know when to eat, how much to eat, and when to stop. I'm sure you've heard your friends talk about diets that they've tried, or said something like, "oh my goodness, Spring Break is 4-weeks away, need to start my cleanse." When you turn on the television it seems like there's a new diet advertisement every day, or a new way to exercise, or some new "miracle pill" that'll melt the fat away. Well, intuitive eating is something that's not a diet, it's a way of life. It's time that we all say "no" to the diets, and start listening to what our bodies are trying to say.
There have been multiple studies showing that restrictive eating does not result in reduced weight in the long term but also, that the majority of individuals dieting to lose weight regain the weight they lost (Mann et al, 2007). Some researchers believe that dieting can actually lead to obesity, due to the mechanism of "yo-yo dieting". If that is the case, then why do so many people continue to do these restrictive diets? Maybe they just need to adopt intuitive eating! I am going to share with you the 10 principles that Tribole and Resch (2012) discussed in their book, Intuitive Eating: A Revolutionary Program That Works.
Reject the Diet Mentality
Rejecting the diet mentality helps people avoid feeling guilty about their meals, let go disordered eating, negative body views, stress, and overall negative relationships with food. The Eat for Life intervention study found that intuitive eating is associated with a positive body appreciation, and that people who live an intuitive eating lifestyle have a lower body mass index (BMI) and make more healthful choices (Bush et al, 2014). Also, studies have shown that post-dieting binges occur in ~50% of all people who end a diet (Tribole & Resch, 2012). You don't have time in college to have an additional stress factor, so ditch the diet mind.
Honor Your Hunger
Hunger is not the bad guy, it's a natural feeling to become hungry, but it's up to you to listen to your hunger cues. As Lauren Outland says, "weight homeostasis does not exist," and we can't fool mother nature (Outland, 2010). When we ignore our hunger cues and proceed to restricting, we may be damaging body chemicals, tissues, and organs. Going hungry causes an increase in ghrelin, an increase in brain hunger chemicals, possible leptin resistance, and metabolism to slow down. Then, once we have the opportunity to eat, we tend to consume more than we would in the first place because we are "starving" (it's an evil cycle). Next time you feel your tummy growling, allow yourself to have a snack, and try not to ignore your hunger cues.
Make Peace with Food
Do you have a favorite food? Sure you do. Now think about that food, do you allow yourself to eat it or do you restrict yourself on how often you eat it? If you tend to restrict yourself from that specific food then think again, and end that war. Stop thinking about what you can and can't have, and learn to fit it into your meals. There's no need to live the majority of your life missing out on the foods we enjoy most, just discover ways to balance your meals, eat some veggies, and maybe get a few extra steps with your friends and family that day.
Challenge the Food Police
See that picture that I first introduced this post with? Well this plays right into that. Our minds have so many things running through it including work, school, money, friend drama, family issues, you name it. Who wants to add another player into the mix? Not I. There is no more of labeling foods, "good" and "bad", because all foods are allowed in your diet. Get rid of that little voice in your head saying, "don't eat that or else this", "can't eat that it's not allowed", "oh that has too much sugar", and the commentary can continue all the way to the check-out line at the grocery store. Don't place all of these food rules in your brain, because I'm sure your brain has enough to think about as it is. Also, if you're concerned about your weight then let me ease your mind. Avalos and Tylka discovered that individuals who responded to their internal hunger and satiety cues on a regular basis tended to be at a weight that is appropriate for their body type, as well as having increased levels of psychological well-being (Avalos & Tylka, 2006). Stop giving yourself another thing to stress about, and enjoy life without the food police!
Respect Your Fullness
Your body is very intelligent, and it is capable of many things, and one thing is knowing when it is satisfied. Listen to the signals your body is sending when you are eating a meal, and understand when your body has had what it needs. Denny et al, looked at intuitive eating in young adults, and they found that women who listened to their body when they were full had lower odds of chronic dieting and binge eating (Denny et al, 2013). When take out all the external cues, and tune in to your internal cues you'd be surprised at what you'll discover while eating.
Discover the Satisfaction Factor
Eating should be a pleasant experience, and it should be a time that you are able to sit down and enjoy the meal that is in front of you. Sometimes we may not all be able to take an hour-long lunch, but for that brief time that you do have, be satisfied with the food on your plate. Augustus-Horvath and Tylka looked at the acceptance model of intuitive eating, and found that individuals who ate mindfully often chose foods that help their bodies function well in addition to being pleasing to their palate (Augustus-Horvath & Tylka, 2011). Eating mindfully doesn't have to be boring, and if you don't like celery then don't eat it. No one forces you to eat things you don't enjoy, and you shouldn't force yourself either. Next time you go to the grocery store have a plan to make a meal that is beneficial to your body along with being appealing to your taste buds. Make meal times a delightful experience, and make it colorful!
Honor Your Feelings Without Using Food
One way that people tend to cope with their feelings is by eating, or better known as "emotional eating". Yes, it's nice to "treat yourself" when you're feeling a bit down, but discover other ways to cope with your emotions other than using food as a reward. Be in-tune with your body, and realize when you are hungry versus bored or upset. Herbert et al found that those who reported practicing intuitive eating were less likely to overindulge in food in the absence of hunger (Herbert et al, 2013). When you find yourself wanting food to help you feel better, think of ways to combat your emotions by not using food as that coping mechanism.
Respect Your Body
We are each created to be special and unique, none of us will have the same body frame, none of us will have the same muscle tone, and none of our bodies will respond to food the same exact way. Learn to appreciate your body, and love the one you have because it's the only one you have. Schoenefeld and Webb discovered that young women who reported higher level of engagement in intuitive eating further reported both higher levels of body image acceptance and compassion as well as being moderate in size (Schoenefeld & Webb, 2013). Another study found similar results, that women with higher levels of intuitive eating are, "more satisfied with their bodies and perceive less pressure to be thin," (Tylka, 2006). Our society is so judgmental and cruel these days, doing way more harm than good, and we need to learn how to ignore what they say and listen to what our body says. Fuel your body with the proper nutrients, let the body do its job, and have self-compassion. Learn to love your body and be comfortable in your own skin.
Exercise - Feel the Difference
Physical activity should be FUN, not a constant misery that you feel is necessary to do 7-days out of the week in order to "maintain your figure". Gastet al, looked at undergraduate women and found that those who were internally motivated to engage in physical activity were also less likely to engage in restrictive eating, and more likely to practice self-care (Gast et al, 2013). This study also showed that increased scores on the Intuitive Eating Scale were correlated with decreases in BMI in both male and female subjects. If we eat intuitively, then our BMI will take care of itself and we won't have to constantly worry about getting those 2-hours of exercise in a day. Try to find ways to move your body that you enjoy, and learn different exercises that your body is capable of doing.
Honor Your Health - Compassion
What you put into your body should taste good, and you shouldn't feel limited to certain foods because in intuitive eating ALL foods are allowed. If you want to indulge, then allow yourself to have that item you desire, because one meal or snack isn't going to break your health. One study on the Health at Every Size program (HAES), found that once the participants listened to their hunger and satiety cues, they were able to regulate their food intake, feel better about themselves, and maintain this behavior change over the 104-week period (Bacon, 2005). They also found that the HAES group saw a decrease in LDL cholesterol and systolic blood pressure, along with sustaining these results at the 2-year follow-up whereas the diet group that was studied did not. Seeing this, it should give us joy that our body knows exactly what to do with the food we put inside of it and once we listen to it, then our overall health will improve as well. Our bodies are truly amazing.
Let's all say good-bye to eating rules, and adapt the intuitive way of eating. Listening to our hunger and satiety cues, enjoying physical activity, nurturing our body with compassion, fueling it with the nutrients it needs, and loving it for all the wonderful things it is capable of. The weight will adjust itself, just trust the process and trust your body. You are wonderfully made, and you are beautiful in your own skin.
References
Augustus-Horvath, C., &Tylka, T. (2011). The acceptance model of intuitive eating: a comparison of women in emerging adulthood, early adulthood, and middle adulthood. Journal of Counseling Psychology. Accessed from
http://u.osu.edu/tracyltylka/files/2015/02/Augustus-HorvathTylkaJCPArticle2buggx0.pdf.
Avalos, L., &Tylka, T. (2006). Exploring a model of intuitive eating with college women. Journal of Counseling Psychology. Accessed from https://www.researchgate.net/profile/Tracy_Tylka/publication/232489009_Explor
ng_a_model_of_intuitive_eating_with_college_women/links/544954650cf2ea65130c1c5.pdf.
Bacon, L., Stern, J., Loan, M., &Keim, N. (2005). Size acceptance and intuitive eating improve health for obese, female chronic dieters. The American Dietetic Association. Accessed from https://naldc.nal.usda.gov/download/8478/PDF.
Bush, H., Rossy, L., Mintz, L., &Schopp, L. (2014). Eat for life: a work site feasibility study of novel mindfulness-based intuitive eating intervention. American Journal of Health Promotion. Accessed from
https://www.researchgate.net/profile/Lynn_Rossy/publication/255910404_E….
Denny, K., Loth, K., Eisenberg, M., &Neumark-Sztainer, D. (2013). Intuitive eating in young adults: who is doing it, and how is it related to disorder eating behaviors? Appetite. Accessed from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3511603/pdf/nihms421703.pdf.
Gast, J., Nielson, A., Hunt, A., &Leiker, J. (2013). Intuitive eating: associations with physical activity motivation and BMI. American Journal of Health Promotion. Accessed from
http://www.morganvanvliet.com/uploads/4/7/5/8/47583769/gast._intuitive_eatingaph.2014_-_annotated.pdf.
Herbert, B., Blechert, J., Hautzinger, M., Matthias, E., & Herbert, C. (2013). Intuitive eating is associated with interoceptive sensitivity: effects on body mass index. Appetite. Accessed from
http://www.morganvanvliet.com/uploads/4/7/5/8/47583769/b.intuitive_eati….
Hudnall, M. (2017). Mindful eating in nutrition counseling for eating behaviors: what research suggests. Today's Dietitian. Outland, L. (2010). Intuitive eating: a holistic approach to weight control. Holistic
Nurse Practice Journal. Accessed from https://www.researchgate.net/profile/Lauren_Outland/publication/4073101….
Jennings, K. (2016). A quick guide to intuitive eating. Authority Nutrition. Accessed from https://authoritynutrition.com/quick-guide-intuitive-eating/.
Mann, T., Tomiyama, A., Westling, E., Lew, A., Samuels, B., & Chatman, J. (2007). Medicare's search for effective obesity treatments. American Psychologist.
Accessed from https://escholarship.org/uc/item/2811g3r3.
Outland, L. (2010). Intuitive eating: a holistic approach to weight control. Holistic Nursing Practice. Accessed from https://www.researchgate.net/profile/Lauren_Outland/publication/4073101….
Schoenefeld, S., & Webb, J. (2013). Self-compassion and intuitive eating in college women: examining the contributions of distress tolerance and body image acceptance and action. Eating Behaviors. Accessed from
https://www.researchgate.net/profile/Jennifer_Webb2/publication/2582513….
Tribole, E., & Resch, E. (2012). Intuitive Eating: A Revolutionary Program That Works. 3rd ed. New York, NY: St. Martin's Griffin.
Tylka, T. (2006). Development of psychometric evaluation of a measure of intuitive eating. Journal of Counseling Psychology. Accessed from http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.541.918&rep=rep1&type=pdf.
How Addressing Stress Can Improve Postpartum Depression
Bethany Edge, Dietetic Intern 2021

When my daughter was born motherhood felt so overwhelming. Looking back, I don’t think it was so much having a newborn, but all the pressure I felt as a new mom to do things a certain way. There is a lot of fear messaging targeted towards new mothers, and this pressure made my worthiness as a parent feel like it depended on following the parenting books to a T.
Like many other women, I found myself experiencing episodes of postpartum depression.
As someone who has battled depression on and off since I was 15, I mentally prepared during pregnancy for postpartum depression (PPD) to hit me HARD. After giving birth, my doctor discovered I had low estrogen. As I began addressing this naturally, I found that many of the same interventions improved my mental health.
I was able to reduce the impacts of PPD by changing my diet, exercising, and reducing stress. Since then I have learned a bit more about why these changes can have such a powerful impact on mental health.
Today I am going to focus on stress, both emotional and physical, and how addressing it can improve PPD.
Things to Keep In Mind
Before I get any further, I want to encourage you to read and apply the following information with a few things in mind.
First, we are all different. There isn’t one approach that can improve PPD for every woman. Individualization is key. Instead of a magical one-size-fits-all approach, I am going to share information that will empower you to figure out what works for you.
Second, recovering from PPD takes emotional work as well as lifestyle approaches.
In my experience, I had to let go of the unrealistic expectations I was imposing on myself and I had to allow myself to get to a place of mental balance.
A counselor can be very helpful, and if you are struggling with PPD, I highly encourage you to seek out a supportive and knowledgeable counselor who can help you.
Finally, recovery takes time. Lifestyle interventions do not work overnight (neither do medications or therapy). It's a process.
In case you need permission, here it is: You have the time and freedom to be on a healing journey. Success is more than just reaching the finish line.
It All Begins with HPA Axis Dysfunction
PPD and depression are complex, but many of the symptoms can be explained by something called hypothalamic-pituitary-adrenal axis or HPA axis dysfunction. The HPA axis is responsible for regulating the body’s stress response along with the sympathetic nervous system (SNS).
Stressors can be almost anything and everything that pushes the body away from homeostasis. They can be internal or external, real or perceived. Either way, they initiate the body’s stress response. Here’s a breakdown of how it works.
- The stress response begins in the hypothalamus, where a stressor signals the release of corticotropin-release hormone (CRH).
- CRH signals the posterior pituitary to release adrenocorticotropic hormone (ACTH) which follows by signaling the release of cortisol.
- While this is happening, the SNS has been releasing norepinephrine which stimulates a “fight or flight response”.
- Cortisol supports the fight or flight response by telling the cells to redirect their efforts towards survival only.
- Once the threat has passed, dehydroepiandrosterone (DHEA) is secreted by the adrenal cortex to counteract cortisol and restore the body to a rest and digest state.
Our bodies are designed to react to occasional stress so we can escape danger. They are also designed to return to homeostasis once the danger has passed (Guilliams, 2010).
Unfortunately, when stress is chronic, our HPA axis may have difficulty working properly and begins to dysfunction.
HPA Axis Dysfunction Can Alter Stress Response
It is well known that stress contributes to the development of many chronic diseases. HPA axis dysfunction may contribute to this by leading to hormone imbalances and organ dysfunction (remember, cortisol tells the cell to focus on survival only. Many important processes may be skipped in this mode) (Guilliams, 2010).
The HPA axis has been linked to depression by multiple studies and in recent years, PPD. In a study of ACTH and cortisol response to exercise stress, women with PPD showed a similar ACTH response to non-depressed women. However, women with PPD were not able to produce the same cortisol response, indicating HPA axis dysfunction (Jolley et al., 2007).
There are four main stressors that lead to HPA axis dysfunction:
- Mental/emotional stress
- Poor sleep
- Blood sugar imbalance
- Chronic inflammation (Guilliam, 2010)
Basically, life with a newborn is a perfect storm.
Here’s the good news! If we can address these stressors, we can improve HPA axis function and postpartum depression.
Managing mental and emotional stressors
As I shared, I believe external stress was a huge contributor to my PPD experience. For many of us, motherhood comes with a lot of pressure. Our loved ones want to support us, but sometimes their words can feel judgmental. There is an unending stream of unsolicited advice about how to give birth, how to feed, or how to interact with our babies.
On top of that, life changes with a baby. Working may become difficult or stressful, friendship dynamics can change, and it may be difficult to do things you once enjoyed now that you’re bringing a baby along.
There are going to be stressors we can control. For example, I decided to throw out my parenting books and unsubscribe to social media accounts that made me feel inadequate. There are going to be stressors we can’t control, like the 16-hour days my husband frequently had to work during the first year and half of our daughter’s life.
I encourage you to identify the stressful things in your life that you can get rid of, and then kick them to the curb. You have better, more important things to worry about, like your beautiful new baby.
For the things you can’t control or avoid, meditation can be a useful tool.
Meditation is reported to improve cortisol levels (Blase & van Waning, 2019). It can seem a little strange and difficult at first, but even listening to a 14-minute guided meditation podcast can improve stress (Basso et al., 2019).
This website has some great meditation tips for beginners if guided meditations aren’t your thing.
Consider finding a meditation routine that works for you and implementing it a few days a week.
Sleep
We all know that sleep is an important part of maintaining a healthy body and mind. It’s one of our most basic needs and not getting enough can put stress on our bodies and HPA axis. I’m sure it’s no surprise that poor sleep during pregnancy and after delivery has been linked to PPD (Okun, 2016).
I know that getting a good sleep with an infant seems like an oxymoron, but bear with me. You have options.
The most basic thing you can do is to begin practicing good sleep hygiene.
Ideally we would all follow a good sleep schedule, but as many new moms know, babies have their own agenda. For this reason, I’m going to avoid the word schedule, and instead encourage you to develop a sleep routine that can be followed any time of day or night to help you unwind.
About 30-60 minutes before bed, take some time to relax, away from screens which can be stimulating. Dim the lights and begin your bedtime self-care routine including brushing your teeth, washing your face, etc. (Suni, 2020).
A great way to relax and improve sleep is to ask your partner for a 20 minute back massage.
A review of non-pharmacological sleep aids in postpartum women found that massage and exercise were most effective at improving sleep. The study also found that when mothers slept better, their infants slept better (Owais et al., 2018).
So if your partner protests, tell them it’s for medicinal purposes.
Practicing yoga during the day or evening can be a great way to kill two birds with one stone as it can be meditative and add physical activity to your day. Thirty-minute sessions 3-5 times a week can help reduce stress and improve sleep (Wang et al., 2020).
As the postpartum period is a time of healing, please talk to your doctor before adding yoga or any other exercise to your routine.
Blood sugar balance
Poor blood sugar control doesn’t just affect diabetics. The standard American diet is high in refined carbohydrates and low in fiber and the result of eating this way is spikes in blood sugar followed by crashes. When blood sugar drops, this can put stress on the body.
Blood sugar imbalance is reported as the number one cause of HPA axis dysfunction (Guilliam, 2010). If you only set one health goal, make it to balance your blood sugar.
There are two key things you can do to improve blood sugar balance. The first is to eat a protein rich breakfast (Park et al., 2015). This has been associated with better blood sugar control in the morning and throughout the day. Turns out there really is something to bacon and eggs for breakfast.
Second, you want to make sure that you are eating plenty of fiber found in whole grains, legumes, fruits, and vegetables. It’s recommended to get at least 25 g of soluble fiber daily, but eating up to 42 g/day has been found to improve blood sugar levels (Silva et al, 2013).
The plate diagram below is a great template for eating for blood sugar balance.
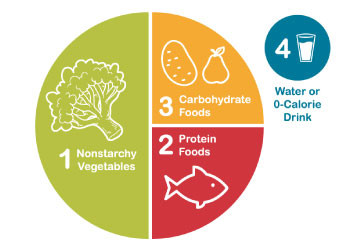
Emphasis is placed on non-starchy vegetables because they are high in fiber and low in carbohydrate. Carbohydrate foods are important and incorporating fiber rich whole grains can be part of a diverse and healthy diet. However, too much of a good thing isn’t good anymore. Emphasizing fiber from vegetables is a great way to increase fiber intake without dumping a huge carbohydrate load on your body.
When it comes to eating for blood sugar control, it's important to take one thing at a time. You don’t need to freak out if you decide to have to eat a piece of cake. The key is to eat in a balanced manner most of the time. Eat foods you enjoy. Eat until you are satisfied. If you want seconds, just grab more of everything to maintain eating in ratio. Be conscious but not obsessive. Remember, we are trying to reduce stress on our bodies. If you balance your blood sugar but are constantly worrying about what you are eating, it just trades stressors.
Inflammation
Addressing inflammation is a big topic, but an important part of healing from depression. Inflammation plays many useful roles in the body, but left unchecked it can do damage to our cells and DNA through oxidative stress. Inflammation can damage the mitochondria (aka the powerhouse of the cell) in our brain resulting in cell death (Bansai & Kuhad, 2016).
Inflammation can also contribute to insulin resistance and poor blood sugar control. It can heighten the immune system and lead to autoimmune diseases. All of these put stress on the body, and you guessed it the HPA axis (Gulliam, 2010).
One way to address inflammation is to improve the balance of omega-3 fatty acids to omega-6 fatty acids in the foods we eat.
Pro-inflammatory, omega-6 fatty acids are essential, but the Standard American Diet is disproportionately high in them and low in anti-inflammatory omega-3 fatty acids. You can increase your omega-3 intake by eating more fish such as salmon or sardines. Omega-3s are also present in walnuts and flax seeds.
Supplementing omega-3s can be beneficial for PPD as well (Mocking et al., 2020). I like Nordic Naturals Postnatal Omega-3. It includes 1120 mg of omega-3 fatty acids plus vitamin D3 which may also help to improve PPD (Amini et al, 2019).
Final Thoughts
Postpartum depression can be overwhelming. Nothing in this article is meant to put pressure on you, so please do not let it add to the stress you are already feeling.
If you don’t know where to start, begin by balancing your blood sugar. It can make a huge impact on your mood.
You aren’t alone. You can reach out for support.
When 10-15% of women experience PPD, there is a good chance you know someone else who can relate and offer support.
Motherhood can be lonely. It doesn’t matter if you stay home, work, or do a bit of both.
There were moments I felt alone in motherhood when I was a stay at home mom and when I was a full time working mom. In those moments, reaching out to others brought me strength and helped me to keep moving forward. Community can make all the difference.
Today I find joy in motherhood. It isn’t always perfect. Some days are much better than others, but I don’t feel that dark cloud of depression constantly looming over me.
Brighter days are ahead, and I know you can get through this!
References
Amini, S., Jafarirad, S., & Amani, R. (2019). Postpartum depression and vitamin D: A systematic review. Critical Reviews in Food Science and Nutrition, 59(9), 1514–1520.
https://doi.org/10.1080/10408398.2017.1423276
Bansal, Y., & Kuhad, A. (2016). Mitochondrial dysfunction in depression. Current
Neuropharmacology, 14(6), 610–618.
https://doi.org/10.2174/1570159x14666160229114755
Basso, J.C., McHale, A., Ende, V., Oberlin, D.J., & Suzuki, W.A. (2019) Brief, daily meditation enhances attention, memory, mood, and emotional regulation in non-experienced meditators.
Behavioural Brain Research, 356, 208-220. https://doi.org/10.1016/j.bbr.2018.08.023.
Blase, K. L., & van Waning, A. (2019). Heart rate variability, cortisol, and attention focus during shaman tha quiescence meditation. Applied Psychophysiology and Biofeedback, 44(4), 331–342. https://doi.org/10.1007/s10484-019-09448-w
Guilliams, T.G. (2010). Chronic Stress and the HPA Axis: Clinical assessment and therapeutic considerations. The Standard, 9(2).
Jolley, S. N., Elmore, S., Barnard, K. E., & Carr, D. B. (2007). Dysregulation of the hypothalamic-pituitary-adrenal axis in postpartum depression. Biological Research for Nursing, 8(3), 210–222. https://doi.org/10.1177/1099800406294598
Mocking, R., Steijn, K., Roos, C., Assies, J., Bergink, V., Ruhé, H. G., & Schene, A. H. (2020). Omega-3 fatty acid supplementation for perinatal depression: A meta-analysis. The Journal of Clinical Psychiatry, 81(5), 19r13106. https://doi.org/10.4088/JCP.19r13106
Okun, M.L. (2016). Disturbed sleep and postpartum depression. Current Psychiatry Reports, 18(66). https://doi.org/10.1007/s11920-016-0705-2
Owais, S., Chow, C.H.T., Furtado, M., Frey, B.N., Van Lieshout, R.J. (2018). Non-pharmacological interventions for improving postpartum maternal sleep: A systematic review and meta-analysis. Sleep Medicine Reviews 41, 87-100. https://doi.org/10.1016/j.smrv.2018.01.005
Park, Y. M., Heden, T. D., Liu, Y., Nyhoff, L. M., Thyfault, J. P., Leidy, H. J., & Kanaley, J. A. (2015). A high-protein breakfast induces greater insulin and glucose-dependent insulinotropic peptide responses to a subsequent lunch meal in individuals with type 2 diabetes. The Journal of nutrition, 145(3), 452–458. https://doi.org/10.3945/jn.114.202549
Silva, F.M., Kramer, C.K., de Almeida, J.C., Steemburgo, T., Gross, J.L., Azevedo, M.J. (2013). Fiber intake and glycemic control in patients with type 2 diabetes mellitus: a systematic review with meta-analysis of randomized controlled trials, Nutrition Reviews, 71(12), 790–801. https://doi.org/10.1111/nure.12076
Suni, E. (2020). Sleep hygiene. Sleep Foundation. https://www.sleepfoundation.org/sleep-hygiene
Wang, W. L., Chen, K. H., Pan, Y. C., Yang, S. N., & Chan, Y. Y. (2020). The effect of yoga on sleep quality and insomnia in women with sleep problems: a systematic review and meta-analysis. BMC Psychiatry, 20(1), 195. https://doi.org/10.1186/s12888-020-02566-4
(n.d). What is the diabetes plate method? Diabetes Food Hub. https://www.diabetesfoodhub.org/articles/what-is-the-diabetes-plate-met…
Ditch the Midol Bottle and End Your Period Pain with These 5 Steps
How I Avoided Painful Period Cramps, Post-Birth Control
Coral Bunch Bassinger, Dietetic Intern 2020

The Untold Secrets of Birth Control
Did you know that over 100 million women worldwide are using birth control? The funny thing is that most of us don't start birth control to prevent pregnancy! Why did you start the pill? Did you have irregular periods, a heavy flow, painful periods, or acne? I started taking birth control when I was 17 years old because I was having irregular periods. The doctor told me that birth control would fix the problem, plus help with my acne. So, as a 17-year-old in high school, I was all in! Little did I know about the problems the pill would cause and the pain that would come from trying to get off the pill later on. A couple of years later, still taking the pill religiously, I began getting anxious, depressed, and I couldn't sleep. I took it for as long as I could, before getting prescribed an antidepressant. Did you know that the primary reason for women getting off of birth control is because of mood changes and depression (Shakerinejad et al., 2013)? If depression and not sleeping weren't enough, a doctor diagnosed me with osteopenia, IN MY 20's. Did you know that the pill can deplete nutrients that are vital for bone strength, and other important bodily functions (Lussana et al., 2003)? But that wasn't the worst part. The worst part was trying to get off of birth control, and not being able to because of the unbearable cramps and pain.
My Story
When I tried getting off the pill for the first time, I couldn't believe the pain. When I started the pill at 17 years old, I had very light and easy periods. That was not my reality anymore, so I ran back to the pill after that miserable week. A year later, I tried again, but this time the pain was so bad that I had to go home from work. I was nauseous, pale, and would sweat from how bad the pain was. I wanted to be off the pill so bad, but I couldn't let my period interfere with my daily routine. It's not like I could just ask off from work every month because of my period. So, disappointingly I ran back to the pill, feeling like a failure and feeling helpless. It wasn't until my third try at getting off birth control that it was a success. My third time of trying to get off birth control was radically different from the times before. I began my master's degree in functional nutrition, and I learned how diet and lifestyle changes can impact so many different diseases and disorders. I attempted this approach with my period pain, and the results were astounding! I have now had a regular period every month, with mild to no cramps, for 9 months in a row! I have learned that although painful cramps are common, they are not normal, and covering up the symptoms with the pill does not solve the issue. Today, I am going to provide you with the solutions that helped me have pain-free periods!
1. Saying "Sayonara" Sugar
About a week before I got off of birth control for the 3rd time, I started to eat a paleo-based diet. This change meant kicking sugar to the curb and any other processed foods. Sugar is a tough ingredient to get away from, I mean, sugar is in salad dressings, soups, tomato sauce, and hidden in many other foods. At first, it was difficult to give up, boy did I have a sweet tooth! But after avoiding sugar and eating whole foods, the cravings began to disappear. Sugar is important to remove from your diet because it increases inflammation in your body, and the process of inflammation leads to pain. There are hormone-like compounds in our body, called prostaglandins, that are very important when your period comes around each month. It is prostaglandins that allow your uterus to contract and release the lining of your uterus (the bloody part) each month. Sugar is important to remove from our diet because it increases the production of prostaglandins, which can intensify inflammation and the pain you feel during your period (Airaodion et al., 2019). One study looked at university students and how their diet was associated with their period. It turned out, that students who consumed a diet higher in sweets, desserts, and junk food, compared to students who consumed a diet high in fruits and vegetables, had a much higher risk for painful periods. The study also showed that fruits and vegetables have a protective role against PMS symptoms, by providing anti-inflammatory and antioxidant effects (Najafi et al., 2018). I found this fact to be true in my own life. I gave up sugar completely for 30 days which turned into a lifestyle change. Don't get me wrong, I still enjoy a nice dessert here and there, but first, I don't crave sugar like I used to, and secondly, having painless periods makes it worth it!
2. Ditch Dairy and Goodbye Gluten
Dairy and gluten (a protein found in wheat, barley, and rye) are common food allergens that can increase inflammation in your body (Soares, 2013; Stancliffe, 2011). I gave up these two common allergens for a month and then reintroduced them into my diet. Eliminating dairy and gluten may allow you to find food intolerances that are leading to more inflammation in your body, which could be exasperating your symptoms.
3. Let Magnesium Work Its Magic
Magnesium plays a significant role in the contraction and relaxation of the uterine wall. It is estimated that 45% of Americans are deficient in magnesium and a whopping 60% of Americans are not consuming the optimum amount of magnesium that we need (Workinger et al., 2018). Magnesium deficiency can cause fatigue, irritability, weakness, and painful period cramps. Magnesium helps relieve cramping by relaxing the muscles (Workinger et al., 2018). One study revealed that girls who did not have painful cramps had higher magnesium levels compared to those dealing with painful cramps. Research suggests that 67% to 90% of women between the age of 17 and 24 struggle with painful periods (Chhabra, 2017). Period pain is very common but is not normal! I was able to end my painful periods, and I want that for you too! On top of eating a diet rich in fruits and vegetables, I supplemented with magnesium glycinate. I take 300 mg of magnesium glycinate every night and I increase the amount to 600 mg a week before my period begins. One study showed that there was no difference between Ibuprofen and 500-1000 mg of magnesium, as a treatment for painful periods (Julie, 2013). Food sources high in magnesium include spinach, squash and pumpkin seeds, lima beans, tuna, brown rice, almonds, dark chocolate, avocados, non-fat yogurt, and bananas, however, it is difficult to consume the amount of magnesium that we need through diet alone, so I found it beneficial to supplement (Whitbread, 2020).
4. Ginger
Afraid that magnesium won't do the trick? Or do you want a backup because of the dread and fear that painful periods can cause? Another remedy to help with painful periods is ginger. Ginger provides anti-inflammatory effects, to help with those miserable cramps. Ginger is a safe therapy to use, it has been used in Traditional Chinese Medicine for thousands of years. One study compared the effects of 1000mg of ginger a day to Ibuprofen, and ginger was found to be just as effective at reducing the severity of cramps in women (Ozgoli et al., 2009).
5. Omega-3 Fatty Acids
Increasing your omega-3 fatty acids is the last step I have to help prevent those miserable cramps from coming around each month. Omega-3 fatty acids are a family of healthy fats that the body needs to function properly. Omega-3 fatty acids are very beneficial in preventing various diseases by helping reduce inflammation. As you can see, it's all about reducing inflammation in the body! Sources of omega-3 fatty acids include salmon, tuna, oysters, firm tofu, flaxseed, chia seeds, and walnuts (Whitbread, 2020). Another important fat that the body needs is omega-6 fatty acids, but problems arise when the ratio between omega-3 fatty acids and omega-6 fatty acids become out of whack. The Western diet tends to promote an imbalance between these two fatty acids and the creation of modern vegetable oils promoted it (Kris-Etherton, 2000). Vegetable oils like, safflower oil, sunflower oil, corn oil, cottonseed oil, and soybean oil, contain a high level of omega-6 fatty acids and little to no omega-3 fatty acids (Kresser, 2019). If you look at the back of pre-packaged foods, these oils are packed into most foods, not to mention fast food uses many of these vegetable oils as well. A couple of ways to reduce the amount of omega-6 fatty acids that we intake is to read the food labels, and to avoid fast food and prepackaged foods, instead, try to consume your omega-6 fatty acids from sunflower seeds, pine nuts, brazil nuts, pecans, and avocados. Studies have shown that too much omega-6 fatty acids can promote inflammation, but increasing our omega-3's, can have the opposite effect (Simopoulos, 2004). One study showed that increasing omega-3's can decrease the severity of cramping during our period (Rahbar, 2012).
Your Turn!
I hope you found this article to be helpful on how to prevent miserable cramps from coming around each month. You are not alone, I know that painful periods are not a joke, but it is not a normal response that the body should be having. I hope that you find relief from your period pain by following these 5 steps!
References
Airaodion, A. I., Adejumo, P. R., Njoku, O. C., Ogbuagu, E. O., & Ogbuagu, U. (2019). Implication of sugar intake in haemorrhoid and menstruation. International Journal of Research and Reports in Hematology, 1-9.
Brighten, J. (2019). Beyond the Pill: A 30-day Program to Balance your Hormones, Reclaim your Body, and Reverse the Dangerous Side Effects of the Birth Control Pill. HarperOne.
Chhabra, S. (2017). Primary dysmenorrhea and serum magnesium in young girls A pilot study. Nessa J Gynecology.
Kresser, C. (2019). How Too Much Omega-6 and Not Enough Omega-3 Is Making Us Sick. Chris Kresser. https://chriskresser.com/how-too-much-omega-6-and-not-enough-omega-3-is-making-us-sick/
Julie, G. (2013). Comparison between magnesium supplement and Ibuprofen as treatments of primary dysmenorrhea and dietary intake of school going girls in Machakos, Kenya: Randomized trial. (Doctoral dissertation, Kenyatta University).
Kris-Etherton, P. M., Taylor, D. S., Yu-Poth, S., Huth, P., Moriarty, K., Fishell, V., ... & Etherton, T. D. (2000). Polyunsaturated fatty acids in the food chain in the United States. The American Journal of Clinical Nutrition, 71(1), 179S-188S.
Lussana, F., Zighetti, M. L., Bucciarelli, P., Cugno, M., & Cattaneo, M. (2003). Blood levels of homocysteine, folate, vitamin B6 and B12 in women using oral contraceptives compared to non-users. Thrombosis Research, 112(1-2), 37-41.
Najafi, N., Khalkhali, H., Tabrizi, F. M., & Zarrin, R. (2018). Major dietary patterns in relation to menstrual pain: a nested case control study. BMC Women's Health, 18(1), 69.
Office of Dietary Supplements. (2020). Magnesium. Retrieved April 15th, 2020, from https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/#h3
Ozgoli, G., Goli, M., & Moattar, F. (2009). Comparison of effects of ginger, mefenamic acid, and ibuprofen on pain in women with primary dysmenorrhea. The Journal of Alternative and Complementary Medicine, 15(2), 129-132.
Rahbar, N., Asgharzadeh, N., & Ghorbani, R. (2012). Effect of omega-3 fatty acids on intensity of primary dysmenorrhea. International Journal of Gynecology & Obstetrics, 117(1), 45-47.
Shakerinejad, G., Hidarnia, A., Motlagh, M. E., Karami, K., Niknami, S., & Montazeri, A. (2013). Factors predicting mood changes in oral contraceptive pill users. Reproductive Health, 10(1), 45.
Simopoulos, A. P. (2004). Omega-6/omega-3 essential fatty acid ratio and chronic diseases. Food Reviews International, 20(1), 77-90.
Soares, F. L. P., de Oliveira Matoso, R., Teixeira, L. G., Menezes, Z., Pereira, S. S., Alves, A. C., ... & Alvarez-Leite, J. I. (2013). Gluten-free diet reduces adiposity, inflammation and insulin resistance associated with the induction of PPAR-alpha and PPAR-gamma expression. The Journal of Nutritional Biochemistry, 24(6), 1105-1111.
Stancliffe, R. A., Thorpe, T., & Zemel, M. B. (2011). Dairy attenuates oxidative and inflammatory stress in metabolic syndrome. The American Journal of Clinical Nutrition, 94(2), 422-430.
Whitbread, D. (2020, April 9). Top 10 Foods Highest in Magnesium. My Food Data. https://www.myfooddata.com/articles/foods-high-in-magnesium.php
Whitbread, D. (2020, April 9). Top 10 Foods Highest in Omega 3 Fatty Acids. My Food Data. https://www.myfooddata.com/articles/high-omega-3-foods.php
Workinger, J. L., Doyle, R., & Bortz, J. (2018). Challenges in the diagnosis of magnesium status. Nutrients, 10(9), 1202.

 Axe ’Em, Jacks!
Axe ’Em, Jacks!