The University of Texas System provides funding for SFA’s Workers’ Compensation Insurance through a self-insured Workers’ Compensation program. The WCI program is administered by UT System through a third-party administrator, Cannon Cochran Management Services, Inc. (CCMSI). Administering the program includes, receiving, investigating and making liability determinations on WCI claims; determining the reasonableness and necessity of medical treatment and services; generating income benefit payments to injured employees when warranted and medical payments to health care providers. All employees on the payroll of Stephen F. Austin State University are covered by The UT System Workers’ Compensation Insurance Program. This coverage extends to student employees.
SFA’s WCI covers on-the-job injuries that occur in the course and scope of employment and that result in damage or harm to the body. It also covers occupational diseases directly caused by exposure in the workplace. WCI can provide:
- Payment of doctor bills, hospital bills, medicine, ambulance and other reasonable and necessary medical care
- Weekly income benefits in the event income is lost as a result of your injury;
- and other benefits as appropriate.
The Office of Environmental Health, Safety, and Risk Management is responsible for coordinating the SFA WCI program. The safety officer serves as a facilitator between all UT System WCI entities and SFA employees who are injured in their course and scope of their employment by submitting the necessary forms and making every effort to negotiate modified duty assignments. Erik F. Santes, safety officer, is the SFA campus WCI representative and can be reached by phone 936.468.4514 or email WCI@sfasu.edu.
Reporting a Work-Related Injury or Occupational Disease
- SFA employees who experience a work-related injury are required to report the incident to their supervisor or someone in a management position immediately after occurrence.
- The injured employee, supervisor or designee is advised to notify SFA's Office of Environmental Health, Safety and Risk Management regarding the injury by filling out the Accident/Injury 24-hour Quick Link Report.
- SFA employees are required to report all injuries/illnesses within 24 hours, even if they do not need medical attention.
Reporting Instructions for Employees
1. Notify your supervisor immediately, no matter how minor the injury may seem. If necessary, report unsafe working conditions to your supervisor or Jeff Thompson at 936.468.6034.
2. If necessary, obtain medical attention. Inform the medical provider that your injury or illness is work related. If it is an emergency, call 911 and get a first responder immediately to the scene. Otherwise, you should seek care from the nearest urgent care facility or hospital ER. However, follow-up care must be received from a network provider. The WCI provider will coordinate all medical care and make referrals for diagnostic testing or specialist appointments.
3. Following the incident, you will be sent to an urgent care facility for medical attention, and a drug and alcohol test will be performed as required by the University's policy on Drug and Alcohol Testing.
4. The system will generate an automatic email notice with the First Report of Injury Packet that you will need to submit to the safety office through email or in person if you were hurt at work and wish to seek medical attention after an injury/accident report has been submitted.
The First Report of Injury Packet includes:
- Employee's First Report of Work-Related Injury or Occupational Disease
- WCI Network Acknowledgment
- WCI Employee’s Leave Election (WCI Form-23)
- RX Bridge Pharmacy First Fill Form
5. The injured employee must complete the Employee’s First Report of Work-Related Injury or Occupational Disease. Complete and sign the WCI Network Acknowledgement form using your physical home address (No PO Box). To determine if you live in a network covered service area. You will find a list of covered counties using the IMO link and instructions below.
- Select a treating physician from the network if you live in a covered service area:
Go to www.injurymanagement.com and search for a provider or call IMO at 877.870.0638.
You must also complete the WCI Employee’s Leave Election form (WCI Form-23) to select the type of leave you wish to use.
The RX Bridge First Fill Prescription Card enables an injured employee to fill prescription(s) prescribed by a provider at the notice of a work-related injury. Employees should tell pharmacies about WCI and provide them with the phone number of the UT System/RX Bridge prescription network (1.833.792.7434), if there are any problems.
Please return the forms included in the First Report of Injury Packet to the EHSRM office at 430 E Austin St. Nacogdoches, TX 75965 or via email at WCI@sfasu.edu.
6. If you miss work due to an on-the-job injury, you must keep your supervisor and the WCI Representative informed of your work status by providing a Division of Workers’ Compensation Work Status Report (DWC-73) after each doctor visit. The doctor’s office must provide this report to the injured employee.
7. When your doctor releases you to return to work, you must report to work at the beginning of your next regularly scheduled shift. The DWC-73 report from your doctor indicating a return-to-work date or any work-related limitations must be given to your supervisor before you may return.
*Important: Remember, If you treat outside of the network without network approval you may be held responsible for medical bills regarding those visits if determined, you live inside a network covered area.
If you are dissatisfied with the network, you may file a complaint by completing Complaint Form #IMO MSN-3. To obtain and submit this form contact IMO by calling 877.870.0638 or emailing them at netcomplaint@injurymanagement.com.
Reporting Instructions for Supervisors or Managers
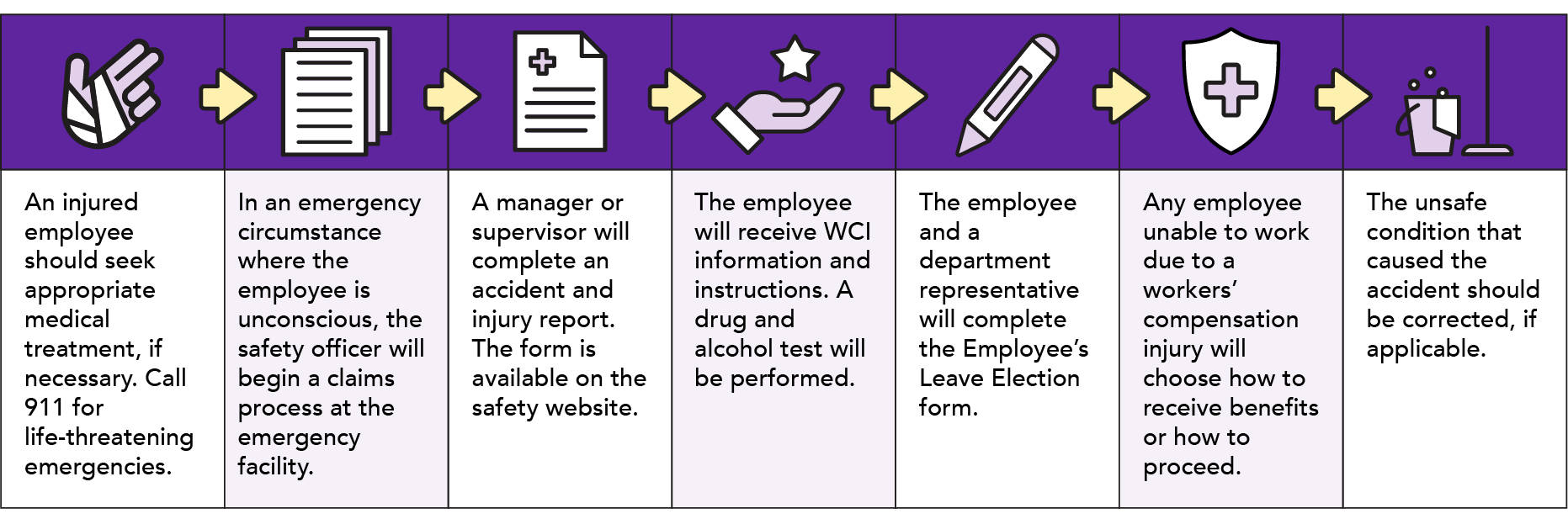
- If the injury is of the nature that treatment is urgent, arrange for appropriate medical treatment. Call 911 for life-threatening emergencies. The employee has the right to select his or her own treating physician. Keep in mind that some physicians do not accept WCI so refer the employee to a Health Care Network Provider. If the employee is incoherent, the supervisor or designee may select an emergency facility. Supervisors or designee shall accompany the employee to the emergency facility to assist with check-in and to provide any details or information to the ER admitting desk.
- In an emergency circumstance where the employee is unconscious, the safety officer will begin a claims process at the emergency facility.
- The manager or supervisor is required to complete an accident and injury report as quickly as possible. The online form can be accessed by clicking the Accident/Injury 24-hour Quick Link on the EHSRM website. If the employee sustained a work-related injury and wishes to receive medical attention following the submission of an injury/accident report, the system will automatically create an email notice with the First Report of Injury Packet for the employee to complete and submit to the safety office through email or in person. The instructions for submitting the forms are located at the bottom of the form.
- If the injury is not an emergency but medical care is required, the injured employee will be contacted by the safety officer during regular business hours, Monday through Friday, 7 a.m. to 4 p.m.. The employee will receive WCI information and instructions. Additionally, a drug/alcohol test will be performed as required by the University’s policy on Drug and Alcohol Testing.
- The employee and department representative must complete the Employee’s Leave Election (WCI Form-23) form. The form is necessary for each period of time the employee has lost time (more than a day/shift due to the injury).
- Employees unable to work due to a workers’ compensation injury, have the option to use their accrued sick and/or annual leave before receiving income benefits. If the employee chooses not to use any accrued sick or annual leave or has previously exhausted all leave, the employee’s status will be leave without pay (LWOP). The employee must be given notice that he or she will be placed under the Family Medical Leave Act (FMLA) from the first day of absence, if the employee and injury are eligible under the law. Call the SFA HR office at 936-468-2304 for more information about FMLA and procedures to follow.
- If applicable, the unsafe condition that caused the injury should be corrected. If assistance is necessary to complete the correction, contact Jeff Thompson at 936.468.6034.
After Medical Treatment
As a workers’ compensation-injured employee you are required to follow all medical instructions and restrictions the doctor has prescribed including follow-up care:
- You will need a work release or work restriction form from your workers’ compensation provider for you to give to your supervisor and a copy to the Office of Environmental Health, Safety and Risk Management. This form should be given to you each time you have an appointment; you will not be released for full work duties without this form.
- The form is called a Work Status Report (DWC-073) and it details the restrictions and limitations of the work duties that can be performed by an injured employee. This form will be the basis of the Bona Fide Offer of Employment (BFOE) you will receive if there is a modified-duty work available.
- If you have been put on restrictive duties, then you will need to work out the task details with your supervisor and Human Resources in accordance with your job description. Once the amended job duties have been outlined you will receive a BFOE if modified-duty is available. Not all departments offer modified-duty and not all job descriptions allow for any kind of physical limitations.
- Once you receive your BFOE, you will either accept the terms or reject the terms. You should understand if you reject the terms of a BFOE, it may impact your Workers’ Compensation benefits.
- This BFOE will be valid until the workers’ compensation doctor modifies the restrictions at which time availability of accommodations will be reassessed. If the accommodations are available, another BFOE will be made.
- If no modified-duty assignment is available and you choose to utilize your sick time, you will be on sick leave until all accrued sick leave is exhausted. Upon exhaustion of your sick leave, you will be provided an opportunity to use some or all of other leave available. When your option is to no longer use available leave you will be eligible for WCI income benefits. Benefits consists of a weekly check at a reduction of approximately 30 to 35% of your regular pay for full-time employees and 40% reduction for those who work part-time to help you get through the downtime until you can return to work. Please note the weekly benefit amount is subject to a statutory minimum and maximum payment.
- If you elected not to use any sick or vacation time and no modified-duty assignment is available, you will be eligible for WCI benefits. However, no compensation accrues during the first 7 days of absence from work due to the injury. If the disability continues for 2 weeks, the waiting period then becomes payable provided the employee was not in a paid leave status for that time. There is a 7-day waiting period before temporary income benefits (TIBs) can be paid, should the disability extend to the fourteenth (14) day after the first day of disability, the carrier will then issue a TIBs payment for the waiting period.
Workers’ Compensation Insurance Forms
- Employee's First Report of Work-Related Injury or Occupational Disease
- WCI Network Acknowledgment (English | Spanish)
- WCI Employee’s Leave Election-WCI Form-23
- Notification of Work-Related Injury or Occupational Illness
- Witness Statement
Other Forms and Resources
- UT System IMO Med-Select Quick Reference Card
- RX Bridge Pharmacy First Fill Form
- WCI Injury Leave for Peace Officers (Form 23P)
- Employer's First Report and Employee's Rights
- Provider Search and Network Service Areas
- IMO Med-Select Health Care Network FAQs (English | Spanish)
- WC ID Card
Notice of Network Requirement Posters and Required Employer Notices
- Notice 6: Workers’ Compensation in Texas (English | Spanish)
- Notice 9: Work-Related Communicable Diseases & WCI Eligibility (English | Spanish)
- Notice of Employee Rights and Responsibilities (English | Spanish)
- Notice of Network Requirements for The University of Texas System (English | Spanish)
- Health Care Network Employee Handbook for UT System (English | Spanish)
Telemedicine Services Information
University of Texas System and State of Texas WCI Policies
- UT System Workers' Compensation Insurance
- Texas Department of Insurance Division of Workers' Compensation
- Texas Workers’ Compensation Act
Helpful Links
- Workers' Compensation Insurance Coverage HOP Procedures 03-220
- Drug and Alcohol Testing HOP Procedures 05-505
FAQs
What is Workers’ Compensation Insurance?
Workers' Compensation Insurance is a type of insurance specifically designed to provide medical benefits and, in some cases, financial payments to employees on the payroll of Stephen F. Austin State University, a member of the University of Texas System who suffer injuries or occupational disease in the course and scope of employment.
In instances of injury arising out of or in the course of employment, the employee is entitled to all medical aid, hospital services and medication reasonably required at the time of injury and anytime thereafter to cure and relieve the effects naturally resulting from the injury. If the employee is in a network service area, treatment must be from a network provider.
In some instances, financial benefits will be available to offset a temporary loss of wage-earning capacity and/or to compensate for permanent impairment due to the injury. Workers' Compensation Insurance is not health insurance, nor does it provide compensation for damage to or loss of personal property.
*UT System employees have specific guidelines governed by Texas Labor Code, Chapter 503.
When does an injury qualify for a Workers' Compensation Claim?
Were you performing the job you were hired for? If the activity falls under the course and scope of your job it will most likely be eligible for workers' compensation.
Examples:
- You were at an out-of-town conference and there was an uncovered electrical cord you tripped over and hurt your knee.
- You were hurt in a car accident driving on official business. This does not include participating in other non-official activities while at a conference (i.e. golfing, jogging and site-seeing).
- You were performing field research studies and got stung by a hive of wasps
- A file drawer was left open and you ran into it lacerating your arm
- Your finger was penetrated by a needle when emptying the trash and you developed Hepatitis C
All the above scenarios would qualify as a workers' compensation injury and as long as you are performing your official job duties, including official business that takes you out of town, you are eligible to file a workers' compensation claim.
When is an injury not eligible for Workers' Compensation?
There are several scenarios that would make a claim ineligible for workers' compensation. These include but are not limited to:
- You are not on the clock but are on campus when you get injured. Coming to and leaving work, lunch break and other breaks, exercising on campus, etc. These are not covered by workers' compensation.
- If you are injured while talking on your cell phone with personal calls or texting while performing your job duties you will be ineligible for workers' compensation. Being on personal calls or texting is not paying attention to your work, is on personal time and increases the chances for injury considerably. If your job requires you to make a phone call or text, stop what you are doing, complete the communication and resume your duties.
- Horseplay: If you are playing around on your job an hurt yourself you will be denied workers' compensation coverage.
- Pre-existing conditions: Often times we have health issues that are manifesting in our bodies that we are unaware of until something triggers the symptoms. If you get hurt on the job and it is determined that the accident was caused by a pre-existing health condition, workers' compensation benefits will be denied or workers' compensation will cover the area that was injured but not the area that shows where a pre-existing condition has occurred.
Examples of pre-existing conditions are:
- You fell on your knee and strained a muscle, however tests show there is arthritis in the knee. Workers' compensation will cover the cost of bringing the muscle back to health but chances are that the knee may continue to be a health issue because of the arthritis. Workers' compensation will not pay for treatment of this pre-existing condition.
- Back injuries can be problematic in that as we age our spine deteriorates but may not be noticed until something happens and it doesn't heal like a younger, healthier back. This is called "condition of life" and again workers' compensation will cover the injury portion only but not any pre-existing deterioration.
How do I file a claim?
Minor injuries:
- All work-related injuries, accidents and occupational diseases, regardless of the severity, must be reported by the employee to his or her supervisor or someone in a management position immediately after occurrence.
- The supervisor will report the injury to the Environmental Health, Safety, and Risk Management office by filling out a “Accident/Injury 24-hour Quick link report”
- If the injury is minor and no medical treatment is required, it will be categorized as an incident-only report.
- If medical treatment is needed, a claim must be filed and the injured employee must file the First Report of Injury packet with the EHSRM Department and receive worker’s compensation information and instructions.
- If the injury is of the nature that treatment is urgent, the employee and supervisor can go to the approved workers’ compensation clinic and may file a claim immediately after receiving medical treatment from the WCI doctor.
- For follow-up medical treatment: If the employee lives within a network service area and needs treatment, the injured employee must obtain healthcare from a WCI network provider. You may go to your own doctor only if your doctor takes workers’ compensation and is a WCI network provider. (If you choose to go to a doctor that doesn’t take worker’s compensation, then you will be responsible to pay for the medical treatment with your own funds and insurance.)
- You will be sent to an urgent care facility for medical treatment and a drug/alcohol test will be conducted following the accident as required by the University’s Drug and Alcohol Testing policy.
- Once the safety officer files the claim you will be contacted by an assigned CCMSI adjuster who will receive, investigate, and make liability determinations on WCI claims. The adjuster will help facilitate claim related medical treatment and services, generate income benefit payments to injured employees when warranted and medical payment to health care providers.
Serious injuries:
- For life-threatening emergencies, call 911 and get a first responder immediately to the scene. Otherwise, you should seek care from the nearest urgent care facility or hospital ER. However, follow-up care must be received from a network provider. The WCI provider will coordinate all medical care and make referrals for diagnostic testing or specialist appointments.
- Supervisors will follow the first responders to the hospital ER to help check-in the employee and provide any details and information to the hospital ER admitting desk.
- Supervisors should, if possible, ask for a drug/alcohol test to be performed on the injured employee to help with the accident investigation as required under the Drug and Alcohol Testing policy. (Note: If the first responders suspect drug or alcohol use, they will usually perform the tests or request a drug/alcohol test be given.)
- As soon as possible the supervisor will contact the EHSRM Department to report the injury and relay the status of the employee and if necessary, connect with the employee’s emergency contact.
- The supervisor will also fill out an “Accident/Injury 24-Hour Quick Link report” located on the EHSRM website.
- If the employee is mobile after they have received medical treatment and have been released by the hospital, they will come to the EHSRM Department, along with their supervisor and fill out the workers’ compensation claim forms. Otherwise, see step 7 below.
- The safety officer will come to the hospital and start the claim process there. If the employee is unconscious or injured to the extent that the employee is unable to understand and follow the claims process, then the claim should be started by proxy with the employee’s authorized emergency contact.
- For follow-up medical treatment: If the employee lives within a network service area and needs treatment, the injured employee must obtain healthcare from a WCI network provider. You may go to your own doctor only if your doctor takes workers’ compensation and is a WCI network provider. (If you choose to go to a doctor that doesn’t take worker’s compensation, then you will be responsible to pay for the medical treatment with your own funds and insurance.)
- Once the safety officer files the claim you will be contacted by an assigned CCMSI adjuster who will receive, investigate, and make liability determinations on WCI claims. The adjuster will help facilitate claim related medical treatment and services, generate income benefit payments to injured employees when warranted and medical payment to health care providers.
What happens if the employee does not want to seek medical treatment for their work-related injury?
The decision to seek medical treatment is up to the employee, so you cannot force employees to go for medical treatment.
Employees are considered to be in full-duty status if they do not seek medical attention. You should keep an eye on the employee's attendance to look for any potential lost time from injuries. Fill out a the Employee’s Leave Election (WCI Form-23) and notify Human Resources if the employee has lost time due to an injury. The employee should be put on Leave Without Pay (LWOP)-Workers' Compensation if they don't want to use their vacation time or don't have any leave available.
How does an employee report an unsafe work environment?
Please call the Jeff Thompson at 936.468.6034 if you think your workplace is unsafe, or you can submit an email to safety@sfasu.edu.
I have questions about my claim. Who can help me?
The University of Texas System has partnered with CCMSI as their third-party administrator for the Workers’ Compensation program. CCMSI claims adjusters work closely with injured employees on each claim.
CCMSI staff can answer questions about your claim. For help with your claim please contact them at 800.252.5059.
What is the new WCI Health Care Network?
- Stephen F. Austin State University enters a 1305 Certified Health Care Network (HCN), effective September 1, 2023.
- All new injuries that fall within the Injury Management Organization, Inc., Med-Select Health Care Network coverage area are required to treat within the network.
- You can view the “provider search” at www.injurymanagement.com
What is Injury Management Organization, Inc. (IMO)?
IMO is a Certified Utilization Review Agent (URA) and the parent company to the IMO Med-Select Network®. IMO provides Case Management, Pre-Authorization, Medical Bill Review, Industry Care Programs, along with other health care management services.
How do I find out more about the IMO Med-Select Network®?
- Visit the IMO website at www.injurymanagement.com
- Write to: IMO Med-Select Network®, P.O. Box 260287, Plano, TX 75026
- Call the Network Main Line: 214.217.5939 or 888.466.6381
- Call the Customer Care Line: 214.217.5936 or 877.870.0638
What if I have an emergency?
As defined by the Texas Insurance Code:
A medical emergency is the sudden onset of a medical condition manifested by acute symptoms of sufficient severity, including severe pain, that the absence of immediate medical attention could reasonably be expected to result in:
- placing the patient's health or bodily functions in serious jeopardy, or
- serious dysfunction of any body organ or part.
If you need emergency care, you may go anywhere. If you become injured after business hours and it is not an emergency, go to the closest urgent care health care facility.
Except for emergencies, if you are hurt at work and live in the network service area, you must choose a treating doctor from the list of network doctors.
What if I treat outside of the Network?
If you treat outside of the network without network approval you may be held responsible for medical bills regarding those visits if determined, you live inside a network covered area.
What if we are traveling out of Nacogdoches County for work related activities?
In these scenarios if you have a need for emergent care for the injury, please treat at the nearest urgent care or hospital.
Please let urgent care be your first option versus an emergency room if your injury is less severe.
Once you return to your home destination and determine you need more medical treatment you will then need to set up care with a treating doctor in the Nacogdoches County area.
What if I want to change my treating doctor?
The injured employee may change from their initial choice to an alternate choice of treating doctor by notifying the network (TCM). The network will not deny a selection of this one (or ‘alternate’) change of treating doctor through the network.
After the change to an alternate treating doctor, if the injured employee is still dissatisfied, he or she must request and receive permission from the network to change treating doctors.
What is Telephonic Case Management (TCM)?
A Telephonic Case Manager (TCM) is a licensed and certified medical professional that will help coordinate the medical services that your physician recommends. The TCM will also provide education and help with communication between all parties. This individual will contact you via phone and email to discuss your work injury with you.
TCM will assist with:
- Medical Assessments on all Lost Time Cases
- Manage Medical / Retrieve Medical
- Medical Only Case – Medical Recovery
- Treating Doctor Oversight
- RTW Oversight
 Axe ’Em, Jacks!
Axe ’Em, Jacks!